KEY TAKEAWAYS
- By 2025, healthcare will face a shortage of over 731,000 jobs.
- Even the most advanced AI tool possesses limited intelligence.
- Extrapolating AI at its infancy could transform clinical care and alleviate the healthcare labor shortage.
We regret to inform you that this article has not been written by robots. Until then, we have three artificial intelligence (AI) predictions we believe are destined to come true in healthcare. We expect these changes will improve healthcare’s quality, lower costs, transform specialty care, and redefine care delivery. And, we think these changes will be dramatic. What’s more, they will have to be: With a big deficit of healthcare workers just around the corner, the advent of AI will quickly become a question not of if (or even when) but of how fast.
EXHIBIT 1
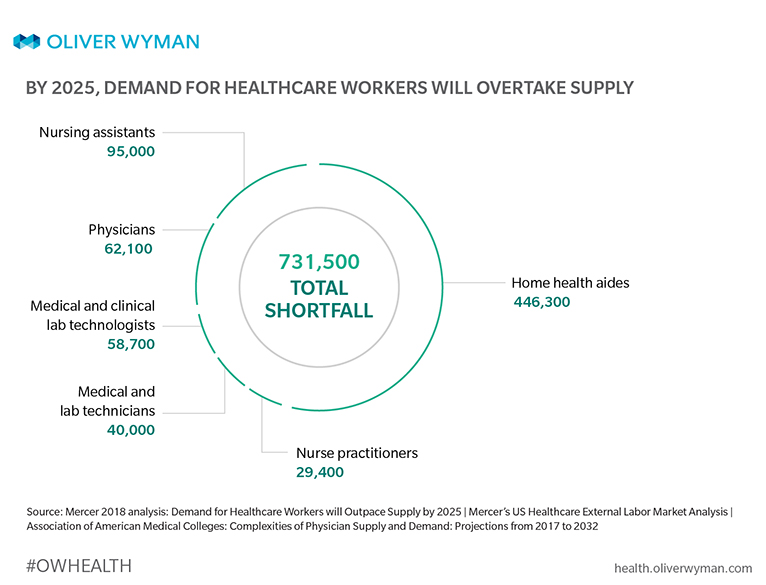
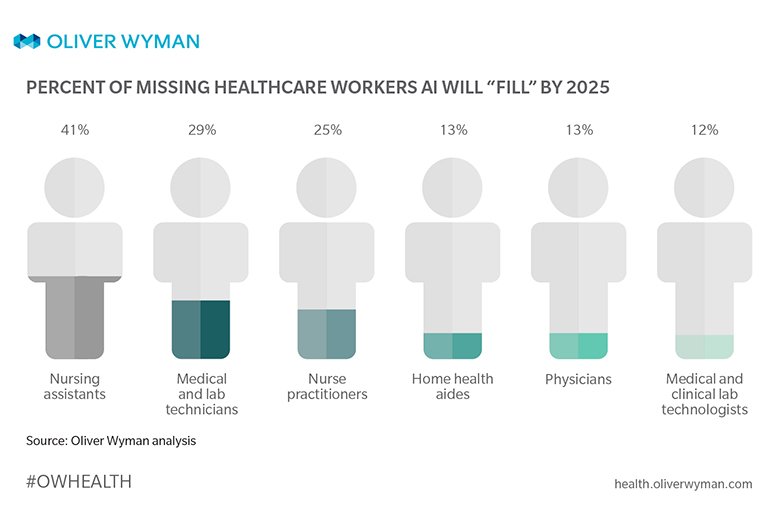
EXHIBIT 2
Because of this healthcare worker shortage, some US hospitals with patient populations dominated by the older, the sicker, and the inactive are even closing their doors. But this isn’t just about a shortage of healthcare workers – it’s instead about a dearth in talent affecting the sector. According to analyses conducted by Mercer and the Association of American Medical Colleges, by 2025 – the year the World Economic Forum predicts machines will do half of human workers’ tasks, no less – healthcare will face a shortfall of more than 731,000 total jobs – including roles like doctors, surgeons, nursing assistants, nurse practitioners, lab technicians, and home health aides.
CUE HEALTHCARE’S ULTIMATE COUPON: AI
Talk of robots replacing human doctors misses the point. When it comes down to it, even the most advanced AI tool is extremely limited, knowing a great deal about a very narrow area of knowledge – kind of like if someone could recite every work of Shakespeare from memory but didn’t know Shakespeare’s first name. Humans, in contrast, know a little bit about many different things – like if a doctor knew how to chop garlic, how to perform heart surgery, and how to write in iambic pentameter. The combination of people and machines, however, is where we see change happening first and fastest. We’ve seen this across countless industries – like when accountants transitioned from ledgers, to adding machines, to spreadsheets, from manual to fully automated assembly lines.
But will this play out in healthcare, or is healthcare just…different? We see a significant opportunity. Extrapolating AI at its infancy could have a transformative impact on several areas of clinical care, and even with a conservative view, could make upwards of a 20 percent dent in the industry’s current labor shortage. These changes are already here, they’re real, and we believe they’ll scale quickly.
AI will transform diagnostic review and optimize testing pathways, slashing volume and waste while delivering faster, more accurate results.
PREDICTION 1 | The Decisive Diagnostician
We predict AI-based radiology solutions will significantly transform radiologists’ diagnostic workflow, “filling” the equivalent of nearly 2,500 radiology workers by 2025. The solutions will also streamline diagnostic workflows of anatomic / clinical pathologists, opthalmologists, dermatologists, and cardiovascular physicians - ultimately "filling" over 2,800 other specialty physician jobs by 2025.
Case Study 1. In 2018, 118 out of 1,000 people in the US – nearly 350,000 – had a magnetic resonance imaging (MRI) scan. In 2025, it’s estimated over 40 million MRIs will be conducted. When an MRI scan is conducted without AI, the process takes about 50 minutes – about 5 minutes to explain an MRI to the patient and another 45 minutes to conduct the procedure, including time spent making sure the machine is physically positioned correctly to acquire necessary images and read the results that come in. With AI-assisted image capture, where much of the process is automated, everything from start to finish takes about 10 minutes. This translates to at least 1.4 billion minutes – or 24.3 million hours – saved in technologists’ time.
Case Study 2. AI’s potential to streamline and transform radiologists’ and specialty physicians’ jobs (such as time spent on diagnostics) is not only notable – it’s measurable. With over 27,500 radiologists currently practicing in the US, and another 540 anticipated to practice in 2025, it’s expected AI will benefit all practicing radiologists’ day-to-day workflows by 2025, about one- third of ophthalmologists’ and dermatologists’ workflows, half of cardiovascular-disease physicians’ workflows, and 90 percent of anatomic/clinical pathologists’ workflows by 2025.
AI will transform nurse practitioners and assistants from skilled craftsmen relying on experiences and skills to customizers of person- centric interventions.
PREDICTION 2 | The Documentation Assistant
We predict AI-based tools will help close the nursing assistant shortage gap by 41 percent, “filling” at least 95,000 new jobs by 2025. And that technology will also “fill” nearly 7,500 nurse practitioner jobs by 2025.
Case Study 1. Nursing assistants spend a reported 50 percent of a typical shift on patients, but the other half is spent on administrative tasks like documentation, writing out care plans, completing admission/discharge/medication paperwork, and transcribing orders. Over a quarter of their day on average – 27 percent – is spent documenting things, 16 percent on care coordination (like communicating with internal and external organizations), five percent on indirect patient care (like reviewing documentation or planning care), with the rest (about two percent) spent on patient education. But AI-assisted clinical data review and documentation means nursing assistants could get back seven percent of this time – that’s the equivalent of over 95,000 nursing assistants coming onto the workforce between now and 2025, according to Mercer analysis.
Case Study 2. The average nurse practitioner spends over half of his or her day – 53 percent, or about six hours – working with electronic health records. Estimated AI documentation savings come to at least 10 percent. With over 142,000 nurse practitioners in 2025 benefiting from these efficiencies, AI would have "produced" the equivalent of 7,500 new nurse practitioners.
Each year, one in three patients is sent to a specialist, with specialist visits making up over half of all outpatient visits. AI will replace the reactive-responsive healthcare worker with predictive-proactive interventions that manage and monitor a patient’s longitudinal health.
PREDICTION 3 | The Downstream Work Eliminator
We predict AI will identify interventions early and eliminate inefficient downstream work currently being done by surgical specialists – closing the labor shortage gap by an additional five percent.
Case Study 1. Patients in need of diabetic retinopathy screening won’t have to visit eye doctors for their annual exams as separate from their annual primary care checkups anymore, thanks to primary care tools built on AI. Instead, they’ll do both at the same time. Of the 23 million diabetic adults in the US, about 48 percent get an annual eye exam. A reported 85 percent of optometrists and 15 percent of ophthalmologists perform these visits. In the future, ophthalmologist capacity should increase when software such as Idx-DR (an AI diagnostics software program that analyzes retina pictures to determine diabetic retinopathy) is used for screening in primary care.
Case Study 2. Surgical site infections (SSI) are the biggest and costliest cause of infections for hospital patients. But AI models can predict which surgeries are most likely to be associated with an infection, enabling a surgeon to take additional preventative actions before – not after – an infection happens. These interventions will reduce the number of patients with surgical infections and lower the total amount of time patients spend in intensive care units. Intensivists and nursing assistants therefore will see a bit more hours “gained” from not having to care for this category of patients.
ALEXA, TELL ME WHAT’S NEXT FOR AI
Technology will shift care delivery. Will payers have to find new and different ways of reimbursement? What will tomorrow’s cultural norms look like for consumers? Is AI coming for healthcare’s jobs faster than we thought? When healthcare saves money, time, and energy, then what? One day, a robot may instantly tell us all we need to know. For now, it’s up to us humans to think about these questions – not “someday,” but today.
For more Oliver Wyman Health insights, visit health.oliverwyman.com.
ABOUT THE AUTHORS
- Tomas Mikuckis, Partner, Health & Life Sciences, Oliver Wyman
- David Waller, Partner, Head of Data Science and Analytics, Oliver Wyman Labs
- Aditya Lingampally, Principal, Health & Life Sciences, Oliver Wyman
- Stacey Sloate, Senior Consultant, Oliver Wyman