KEY TAKEAWAYS
- The typical conversation about clinician shortages needs to expand as shifting models of care and the need to innovate change the nature of work in healthcare.
- Companies need to be deliberate in defining the size and shape of their workforce.
- A “no-regrets” posture – embracing technology and investing in talent – can pave the way to healthcare’s workforce for the future.
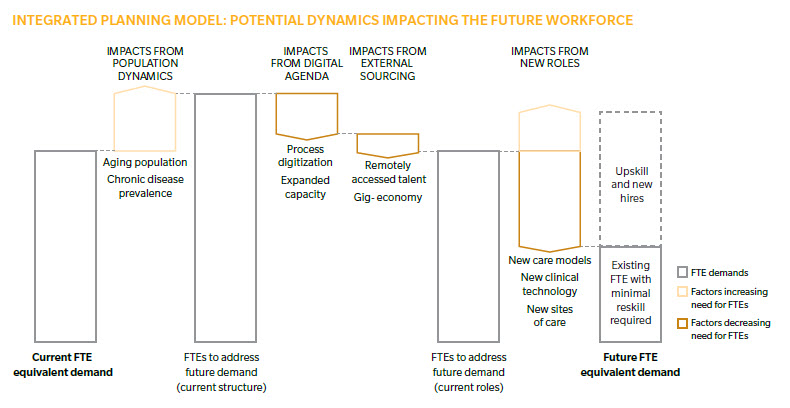
Digitization and automation directly impact up to 45 percent of jobs across industries. As healthcare embraces technology, moves out of the office, and marches toward value, there will be an inevitable need for new roles, smarter skills, and deeper relationships across the workforce. Companies must be deliberate in defining their future workforce’s size and shape. Companies struggle with questions like:
- What changes are impacting my workforce?
- What will my future workforce look like?
- What strategies are needed to bridge from the present to the future?
THE TYPICAL HEALTHCARE CONVERSATION: A SUPPLY SHORTAGE
It’s a familiar complaint echoed across health system C-suites nationwide. Physician dissatisfaction, combined with a dwindling clinical education supply, means an inevitable gap in the ability to deliver care safely and scale businesses.
The numbers support this, with expected shortages of 100,000 physicians by 2030, and shortages for other clinical and non-clinical professions potentially even worse. (Expect a shortage of over 100,000 nurse practitioners and nurse assistants and a dearth of more than 400,000 home health aides by 2025.) While the gaps will differ by state, and even by town, hospital and health system administrators will struggle over the next decade to staff key positions in an environment of cost constraints.
A BROADER HEALTHCARE DIALOGUE: MEETING SHIFTING DEMAND
An aging population, rapidly changing consumer expectations, and the shift toward value-based care demand new skills, new roles, and new interactions between talent. New ways to work, driving innovation and experimentation, will permeate clinical and non-clinical staff. Here are four examples of trends that imply a workforce in healthcare very different from today’s:
- A move out of the office, driven by convenience for consumers and a move toward less costly sites of service, requires an entirely new set of skills to deliver care across different settings. Health providers will need to operate in non-traditional locations and use technology to access and integrate care, engaging patients in unique ways as consumer expectations evolve.
- The shift to value and new models of care requires a more holistic view of consumers and patients. It also demands new roles. Care teams require social workers, population health managers, and many other roles and skills (such as nutritionists and behavioral health) that aren’t common across the healthcare landscape. Further, coordination of care requires differently structured, technology-enabled, and executed relationships between clinicians, managed-care organizations, and community organizations that remain weak as a whole today.
- Scientific advances in fields such as genomics and behavioral science create significant unknowns, for which there is no workforce supply model as of yet. As we shift from reactive to preventive interventions, new roles such as epigenetic counselors will become mainstream. An entirely different set of skills – skills that, at the moment, do not exist, except conceptually – will be necessary to interpret and integrate these new technologies.
- The need to innovate quickly. As new entrants appear in the healthcare space with increasing frequency and intentionality, current business models are increasingly threatened. Experimentation and co-creation need to happen in more rapid cycles, with new skills stemming from being able to anticipate what’s next. Workers will require a bias to act (in stark contrast to today’s bias for long planning cycles) and will need a framework and culture to deal more comfortably with ambiguity and risk.
Given the need for new roles and new skills, we estimate over 50 percent of the workforce could have roles that are significantly modified from today.
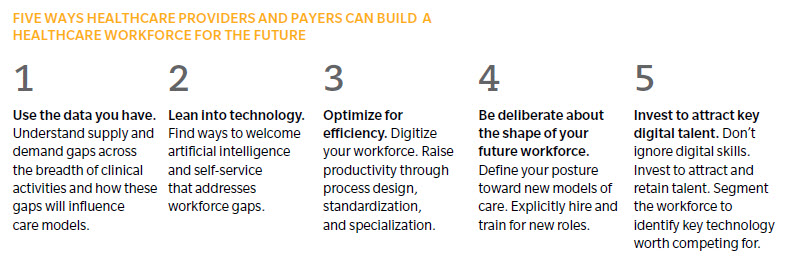
WANT TO STAY AHEAD OF THE CURVE? EMBRACE A “NO REGRETS” POSTURE.
Keeping a finger on the pulse of technological, industry, and sociological trends impacting the workforce is critical to define the size and shape of an organization’s workforce for the future. Technology can be a catalyst to increase capacity, reduce administrative burden, and augment and enhance human capabilities. Here are five ways to stay ahead of the curve.
About the Authors
Chris Schrader is a principal in Oliver Wyman's Health & Life Sciences practice.
Helen Leis is a partner in Oliver Wyman's Health & Life Sciences practice.
Matthew Stevenson is a partner at Mercer.