Despite well-publicized departures from Medicare’s Pioneer ACO Program, the number of accountable care organizations (ACOs) continued to rise last year, though at a slower pace than in 2013. Almost 70 percent of the U.S. population now lives in localities served by ACOs, and 44 percent live in areas served by two or more.
The total number of ACOs participating in Medicare programs has increased to 426, up from 368 in January 2014 and 134 in January 2013. Oliver Wyman has identified an additional 159 ACOs, bringing the estimated total to 585, up from 520 in January 2014, and 260 in January 2013.
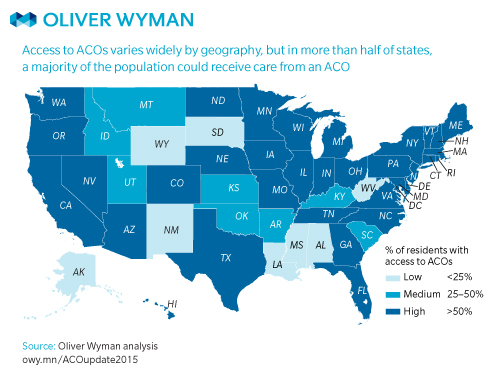
Accountable Care Within Reach: Access to ACOs by State, January 2015
Access to ACOs differs considerably by state—and within states—but in our most recent analysis, a majority of the population in more than half of the U.S. could receive their care from an ACO.