Editor’s Note: The following article is part of an ongoing series offering our strategic advice and expertise on what healthcare industry stakeholders should do in response to the rapidly evolving novel coronavirus (COVID-19) pandemic.
COVID-19’s financial toll is beginning to reveal itself. Many health systems are seeing revenues slashed in half and supply costs surging. There’s uncertainty about when and how quickly service volumes will return. Health systems and the provider community will especially be impacted economically and financially for years to come.
In the meantime, early impacts are startling. Consider, for example, that the Mayo Clinic projected a $3 billion revenue shortfall in 2020 and is expected to experience a $2 billion loss this year. In contrast, last year, they broke a financial record with nearly $1 billion in operating margin.
News like this hits at a time when things like employment, consumer preferences, and where and how people receive care are all being turned upside down, and quickly so. The future of what a post-pandemic landscape holds means a return to the status quo operating model is not a viable future option. Hospitals and health systems must systematically re-think operations and transform their business models.
Navigating the Pandemic
Once the curve has flattened, health systems must solve for their economic challenges in three steps:
- Regroup and restart. First, it’s about restarting the system and tailoring operations to serve both COVID-19 and non-COVID-19 patients.
- Bounce back. Second, it’s about stabilizing the system by recovering core services and case volumes. And, it will be about establishing a cadence toward normalcy.
- Adapt to change. Third, it’s about sustainability and preparing for growth amidst a “new normal.” And, it will be about building a lower-cost operation and operating model that is resilient and can handle potential future market shocks.
Across these three steps, there will be a tangible and necessary focus on near-term results. These metrics include how you’re building back revenues and managing supplies and costs. But long-term sustainability demands scrutinizing every operating model component and imparting necessary operational changes that fundamentally re-envision cost as an investment.
Before attention is placed on longer-term transformations, most health systems will be forced to immediately implement cost containment measures. Two primary levers here include labor (for example, hiring freezes, staff furloughs, freezing or decreasing salaries, and delaying start dates, early retirements, and sabbaticals) and liquidity (for example, federal relief funds, revenue cycle, management of payables, and temporary cost reductions).
Beyond this, providers may choose to take other actions like borrowing, taking out lines of credit, and/or liquidating investments. Although necessary, actions like these won’t put an enterprise on a firm footing. Ongoing liquidity challenges are expected in the long-haul of virus suppression and re-emergence.
In the meantime, providers must learn from other industries’ liquidity crisis management practices. Perhaps, for instance, providers can set up a liquidity management office to continuously monitor and scenario plan cash sources and uses, align leadership on what actions they will take and when, and industrialize a liquidity playbook to weather new spikes in confirmed cases.
Also, providers must consider making fundamental changes to their operations and operating models to achieve new levels of clinical and administrative efficiency and effectiveness.
Pursuing Sustainability
How much cost must really be taken out? Looking ahead, once we get over this initial peak, the next stage will be very challenging. Top-line revenues will face pressure as unemployment, a deteriorating payor mix, and shaken consumer confidence weigh heavily on the recovery of volumes. Further, patient preferences are shifting. Virtual care is accelerating. And it remains to be seen how this pandemic transforms attitudes and behaviors toward hospital-based care.
The few systems that transform their cost structure and improve their cost position by between 10 and 15 percent of their operating baseline are poised to weather the storm.
Consider, for example, the impact of unemployment on health system revenues. Oliver Wyman’s research estimates that a one percent increase in unemployment can equate to between 0.5 percent and over one percent decrease in revenue for providers dependent on commercial payers. With estimated unemployment rates ranging between 10 and 30 percent, the provider outlook is potentially quite severe. (Note that this range assumes providers with commercial rates between 150 percent to 250 percent of Medicare rates and is meant to be an estimate as the actual number will depend on things like whether the unemployed will purchase individual insurance, the payor market dynamics, and provider market share and asset mix.)
This implies that most health systems are likely to turn their narrow operating margins (which average between two and three percent) to significant losses. Incremental cost reduction efforts will be insufficient; what’s essential instead is embracing a mindset shift.
Some may say this approach is one that’s been talked about before. Indeed, cost and operating model transformation have long been critical strategic imperatives for health systems. However, many will also concede these efforts have yet to transform cost structure.
Changing operations and clinical processes involves questioning the status quo, making trade-offs, and implementing strategic choices. It’s about leveraging one collective system as a thriving organism. It’s about portfolio management at the service line level and relentlessly pursuing the most effective, efficient sites of care. It’s about applying business process redesign to remove waste and unnecessary complexity. It’s about building a resilient health system with cost flexibility that is variable whenever possible. And, it’s about creating an operating model that sustains these changes.
The few systems that transform their cost structure and improve their cost position by between 10 and 15 percent of their operating baseline are poised to weather the storm.
Every Dollar You Expense is a Dollar You Can’t Invest
Investments must allow providers to deliver safe, affordable, and high-quality care. Most activities outside of this core must likely be viewed as a commodity service secured at a cost that is competitive in the market.
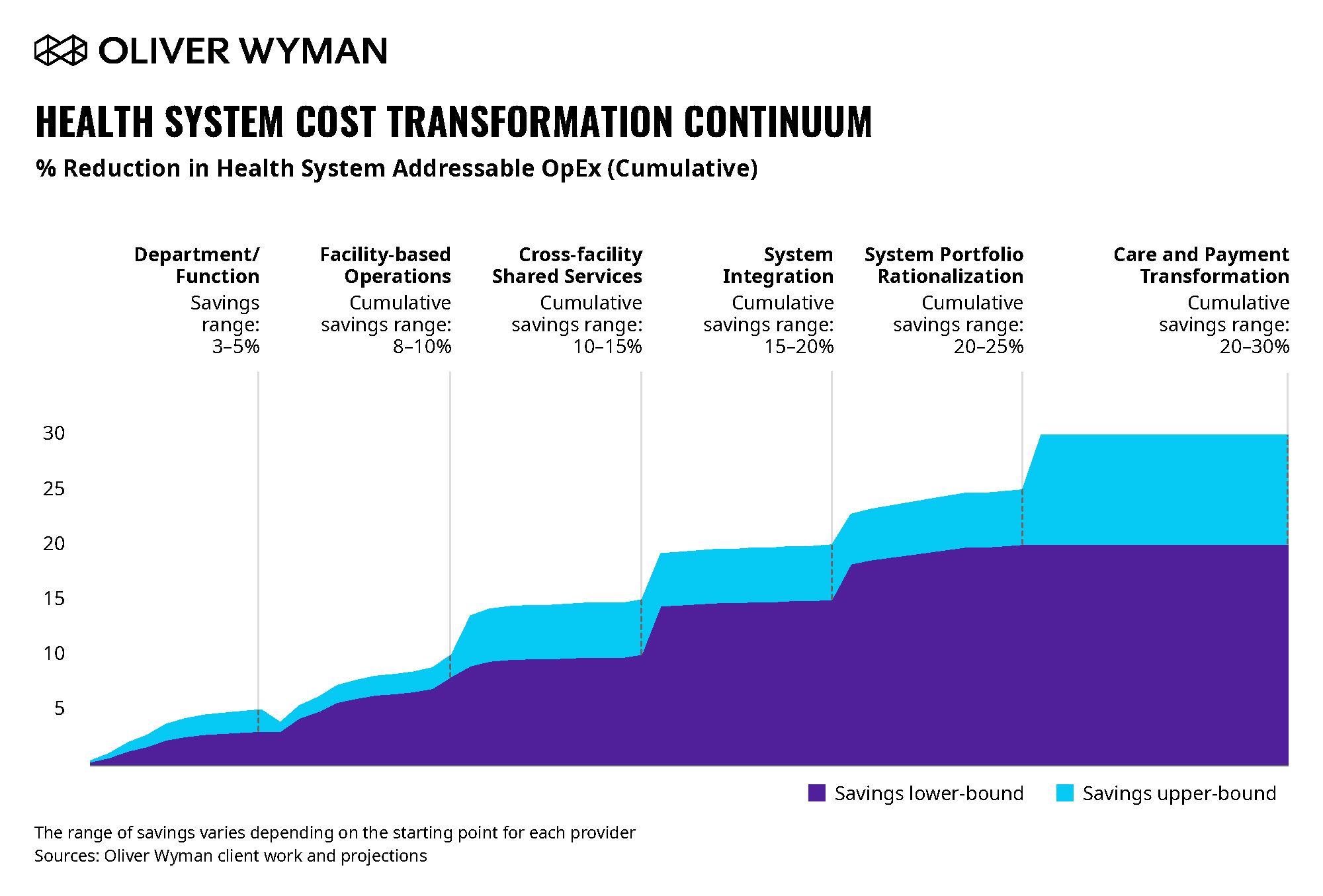
Figure 1 above shows the continuum of cost reduction moving from incremental changes toward full transformation with a vertically integrated care and payment model. Most health systems to date have addressed cost at department- and function-levels, saving three to five percent of their operating baseline by applying benchmark-driven evaluations and taking out costs without changing operations. And, therefore, they’ve operated without prioritizing and removing unnecessary work along the way. As a result, many frustrated health systems can’t sustain cost savings once their costs start creeping back in.
Successful health systems will holistically examine their cost structure, develop an operational blueprint, and establish an operating model that positions them as a system instead of fragmented assets. Acting as a system will allow a more sustainable cost position and will strengthen how you capture gains from specialization. It is only through these actions that health systems can build enough resiliency to sustain in an environment where the government becomes the more dominant payor.
COVID-19 may ultimately transition our healthcare system away from the status quo towards the more sustainable and affordable model we’ve long been trying to build.