The message from state and federal regulators is intensifying: Addressing health equity is no longer a choice for insurers, it is a part of doing business with Medicare and Medicaid. A growing number of states now mandate that insurers incorporate capabilities for tackling health equity in their proposals to become Medicaid managed care organizations. The requirements include creating a chief health equity officer position, developing a health equity plan that’s updated annually, and meeting specific quality measures (Oliver Wyman recently supported Pennsylvania’s Department of Human Services implement the governor’s executive order to address health equity).
At the federal level, the Health and Human Services Department put a stake in ground in April with its Health Equity Action Plan, stating that equity will be a major factor in decision-making going forward. Following that lead, the Centers for Medicare and Medicaid Services in a proposed rule around expanding access and affordability in Medicare Advantage and Part D asked stakeholders for comments on adding a Health Equity Index to its Star Ratings. Future rulemaking would be needed to make that happen, but in its final rule, the agency suggested that an index would help support efforts to address disparities.
And it is worth noting that most providers polled by the Institute for Healthcare Improvement ranked addressing health equity as one of their top three priorities.
Yet when confronting health inequity, many healthcare players do not know where to start. Health inequity is as complex as the very fabric of our society: it is manifested through complex disparities beyond healthcare such as unequal access to education, racial and income inequalities, and other factors that ultimately impact access care. People are not entering the healthcare system on equal footing; this means that one-size-fits-all treatment, while technically “equitable,” will not address existing disparities. With mandates and incentives changing, insurers need a strong foundation to build on as they embed health equity across the enterprise.
Where to start: Building core health equity infrastructure
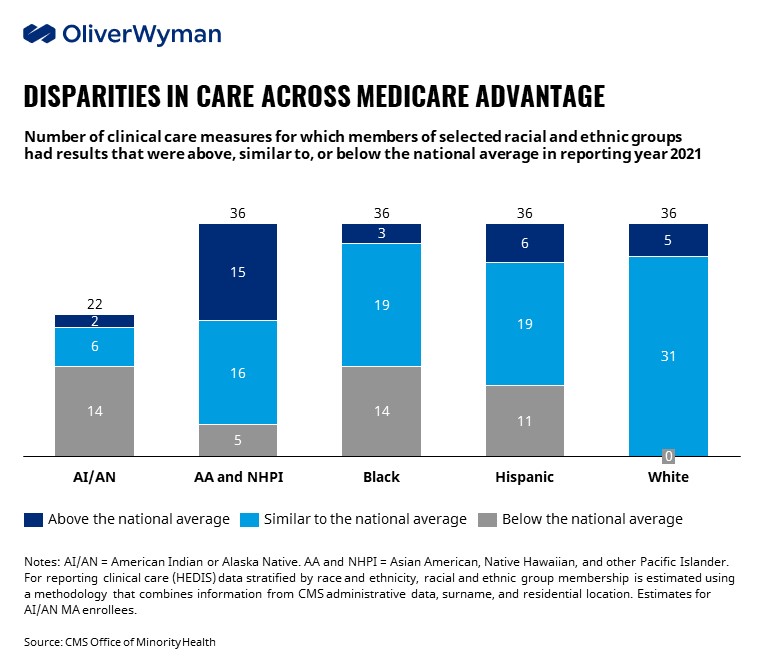
The adverse impacts of health inequity have been apparent for years, especially to those who serve vulnerable populations. The COVID-19 pandemic further highlighted the stark disparities when it comes to access, affordability, and outcomes related to health. Death rates for Black Americans were 441 per 100,000 between 2020-2022, and 466 for Hispanics and Latinos, compared to 268 per 100,000 lives for non-Hispanic Whites. These trends and others have generated a renewed sense of urgency in addressing entrenched structural issues that have plagued the industry for years. The chart below, for instance, shows gap that exists in quality of care within MA plans.
Insurers should start with these no-regret moves as they build out their capabilities:
- Collect data: If you don’t know your members or patients, it will be difficult to address their needs. At minimum, healthcare organizations can start collecting Race, Ethnicity, Language and Disability (REALD) data during enrollments, health risk assessments or any other member interactions. While state agencies are starting to collect this data on Medicaid members, plan and provider representatives can be front-line champions for collecting this information.
- Analyze outcomes and access across different groups: Stratifying members and assessing trends is the first step in recognizing disparities, and regulatory bodies are increasingly incentivizing this behavior. Hawaii, Louisiana, and Nevada are among the states requiring MCOs to stratify disparities data. CMS in April issued its first report highlighting disparities in Medicare Advantage. And in its 2023 proposed rate setting rule, the agency called for insurers to report select Star measures by race and ethnicity. As noted above, the agency hinted at its aim to develop a health equity index to enhance Star ratings for CAI and CAHPS measures and incentivize plans to reduce disparities via care improvements.
- Reflect the members you serve: Members tend to be more involved with their care if they interact with providers and health insurance personnel who can implicitly understand their needs. Multiple studies have shown that provider diversity improves patient health outcomes and organizational performance. Similarly, health plans can foster connectivity and trust with members by ensuring networks include providers with diverse backgrounds and building diverse customer service and care management teams internally.
- Create communications that meet members where they are: The National Assessment of Adult Literacy has consistently shared that those from different cultural backgrounds and those who do not speak English have lower health literacy. Further, these populations were twice as likely to report having poor health. Healthcare organizations can play a critical role in addressing this disparity by ensuring printed collateral and other communications are available for all members, especially those who do not speak English and/or have physical limitations (e.g., impaired hearing). This became especially pronounced with the growth of telemedicine during the pandemic. HHS’ Office of Civil Rights in July issued guidance for ensuring people with disabilities and limited English proficiency have access to quality telehealth services.
Moving beyond the basics: Building member initiatives
Once healthcare players understand member needs and are taking steps to engage them, a core set of questions can help determine where to develop and deploy targeted programs to promote health equity:
- Are you solving for fundamental needs? If an individual doesn’t have access to necessities like food and housing it is unreasonable to expect them to engage meaningfully in managing their medical conditions. The ethnic and racial composition of your population, combined with the geographic footprint, provides valuable insights into where and how persistent such issues are amongst the member population. For example, Highmark is working with the Thrive 18 project to provide residents with health education, housing advice, financial stability, and connects residents to resources that are impacting individual health.
- Do you want to improve access to care? There are glaring disparities along racial lines amongst the uninsured. For example, over 20% of Hispanics are uninsured compared to less than 10% of non-Hispanic whites. While there is acknowledgment of these disparities, more action is needed – insurers and providers can engage with community organizations like National Alliance for Hispanic Health to develop and deploy targeted plans to educate and engage members.
- Do you want to create a support system? Community-based organizations can serve as a key link to achieve quick wins in minimizing health inequities. A recent study published in JAMA found that COVID-19 vaccine hesitancy decreased more rapidly among African Americans compared to non-Hispanic whites when African Americans learned that vaccines were necessary to protect themselves and their communities. Targeted community efforts can be leveraged to address other persistent issues like infant mortality, which disproportionally affect people of color (~8.5 per 1000 amongst African American compared to 4.5 for Caucasians).
Ultimately, there is not a single right answer for where and how address health inequities. It requires a nuanced view into the population you serve, its needs and the objectives and capabilities of the organization.
Results matter, but it’s not just about the ROI
For many players, investment into health equity will involve considering the anticipated impact and return on investment especially the cost of care. Financial returns matter, but these investments are about more than myopic view of the ROI at end of the next quarter or at the end of the year. There is a larger purpose and a greater mission to help challenged individuals get access to the care they need in a fair and equitable fashion.
The healthcare system is immense and complex; paradoxically, it also operates at a deeply individual level. Those with the power to better care for historically underserved population by meeting their unique needs have an imperative to do so. What remains is for stakeholders to understand their members or patients, identify where and how they can contribute, and start now.


