Healthcare workers have not weathered the pandemic well. A strained supply chain, staffing shortages, and endless shifts are among the hardships that took a toll on their wellbeing. Tensions and a lack of trust between executives and front-line workers are also mounting. The result is a chain reaction that impacts access to future care and ultimately threatens healthcare organizations’ stability. More than ever, healthcare needs leaders who are good with people.
That message came through loud and clear during a series of interviews Oliver Wyman conducted with nursing professional earlier this year. An overwhelming majority noted that their employers have historically shown little regard for issues that directly impact wellbeing, like work-life-balance and mental health.
“I left my full-time role because the responsibilities kept piling up and I just wasn’t getting support from the hospital,” one critical care nurse told us. The nursing workforce unsurprisingly desires connection and a supervisor who “has their back” and will advocate for them, but the culture of many healthcare organizations has failed them. This situation has been brewing for a while. Healthcare workers’ perceptions of leadership and whether the organization has a strong support system are predictive of staff retention. In a 2018 Health Resources and Services Administration survey, 20% of nurses who quit their jobs did so due to a lack of good management or leadership. And 29% who stayed with their organization but switched roles cited poor management as a reason for making the change. The situation is more dire now with 60% of front-line workers saying they would not recommend their profession to a family member, according to recent Oliver Wyman survey.
That lack of confidence in leadership showed up throughout the pandemic, hospitals reporting critical staffing shortages. To fill the gap, many turned to temporary staffing agencies, which comes with a host of financial, training, and cultural difficulties. A recent American Hospital Association report noted that travel nurses accounted for 23% of total nurse hours in January 2022, but nearly 40% of labor costs. The AHA also found a 213% increase in hourly rates charged by staffing agencies from January 2019 to January 2022.
There is an even more fundamental concern: without trust, communication gaps occur and leadership loses touch with the continuous changes necessary to keep systems dynamic and improving. A Joint Commission study found a higher commitment to patient safety, more readies to engage in improvement activities, and better team interactions when leaders are more engaged with front-line staff.
The Solution: Wholesale Cultural Change
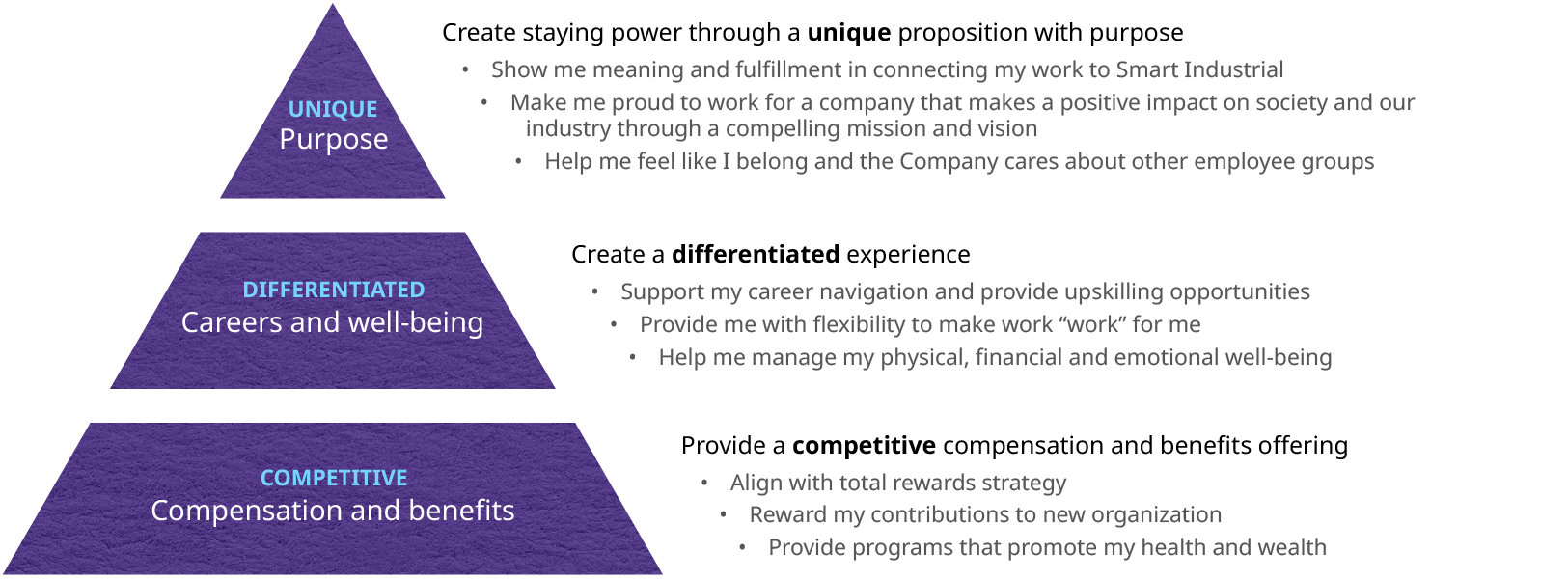
Creating a new value-proposition for workers requires nothing less than a full cultural change. Simply paying more money or carving out a few job perks may work in the short term but will not break the cycle of mistrust and may not even be financially viable for many organizations. Staff today are more concerned with such things as support for mental health and work-life balance.
Healthcare culture has traditionally orbited the twin stars of individualism and altruism. Together, these have bred a form of stoicism. Healthcare is a challenging field, the narrative goes; difficult, even dangerous circumstances are simply part of the job and the solution is for individual workers to simply hang in there and figure it out for themselves. We saw this play out nationwide during the height of the pandemic as front-line staff were forced to contend with shortages in personal protective equipment, taking on extra shifts, and picking up shifts in units for which they weren’t trained. The pandemic also exacerbated the problem of fatigue and burnout. Again, we come back to the issue of leadership. Among physicians reporting burnout, 39% point to a lack of respect from administrators or colleagues as a key cause. Even more fundamentally, the single most important factor in preventing burnout, according to a large scale study by the American Medical Association and the University of Minnesota, was feeling valued by an individual’s organization.
A New Playbook
Leaders need write a new playbook that encourages a more compassionate and systems-level approach to addressing challenges and engaging opportunities for improvement. In the near term, this means reform to several processes and structures.
- See Me, Hear Me, Offer Support: Health systems can build easily accessible formal and informal channels for individuals to make their voices heard. Leaders must be truly engaged in these channels, listening first and foremost, but actively demonstrating their concern and understanding. They can do this by being visible on the front lines, providing the opportunity for informal in-person discussions are critical. More frequent and effective communication has been associated with lower stress and burnout in high pressure ED settings during COVID, and leadership accessibility is associated with everything from lower levers of emotional exhaustion among staff to better patient safety norms. Experimental interventions have further demonstrated this: recent study demonstrated that one-off facilitated communication can help repair relationships between administrators and clinicians. A systematic change to communications could do even more.
- Bottom-up decision-making: Front-line workers, and those from traditionally marginalized groups can feel cut off from the decisions that affect their day-to-day working lives. Formalized structures that provide an opportunity not just for suggestions but for true participation in direction-setting and oversight. Shadow boards are an example of this; a relatively new concept in which front-line workers are empowered to serve on a formalized board that have direct impact on enterprise decision-making. Such structures have improved job satisfaction, trust, and retention.
- Flexibility and agency: This motto for younger generations is rapidly being embraced by the healthcare workforce. While flexibility around scheduling, work locations, and work styles cannot always be achieved, at least for clinical and other in-person roles, healthcare leaders can get creative to offset certain necessary rigidities. For example, nurses can be given the option to rotate within their service lines to try different types of work. Or instead of sticking to rigid, pre-defined roles, nurses’ own preferences and strengths can be considered when determining their day-to-day work to create a greater variety of “majors” within the nursing workforce.
None of this will work without trust. Workers need to believe leadership is doing its best to meet them where they are to accept that it won’t always be able to be as flexible as they might want. Healthcare workers have chosen a difficult path and they are willing to walk it, but they must know that they have as much support as possible and are appreciated and valued for the work they do.
In the long term, even broader organizational changes can solidify the improvement in trust.
Culture: Training, decisions on hiring, leadership promotions, leadership communications content and style, and the other building blocks of culture need to be changed over time to emphasize an inclusive, compassionate, and systems-thinking culture. This is harder than it sounds; it means sometimes passing on short term revenue opportunities or discounting traditional experience advantages to focus on individuals who will contribute to the kind of cultural change that will be long-term beneficial for healthcare organizations.
The New Operating Model: Ultimately, health systems may need to create new roles and reorganize the system to give more frontline workers a say in leadership decisions and create more authority and accountability at the leadership level to improve worker trust.
Examples of this already exist as senior level roles for patient experience and diversity equity and inclusion. While there are already representatives at senior levels for physicians and doctors, it may be time to add a role, or expand the mandate of existing roles to maintaining trust between front-line workers and administrators.
This organizational change may also require new approaches to managing union relationships. Though these relationships are often adversarial, they don’t need to be. Unions can be a partner in providing a voice for employees, and a reason for them to maintain faith in their organization.
Measurable and Meaningful Progress on Diversity in the Workforce: The current healthcare workforce, especially within the nursing ranks, is skewed heavily female. In a perfect world, females’ burdens at home would be no more than their male counterparts, but until that ideal future arrives, the truth is that highly female workforce will be more affected by disruptions to homelife. When COVID closed schools and daycares, that affected women more than men, and thus was particularly impactful for the healthcare workforce. Healthcare organizations should certainly advocate for policies that encourage equitable sharing of childcare and other domestic work and that support families who have those responsibilities. But in the meantime, a more diverse workforce will be a more resilient one.
The deficit in trust between front-line healthcare workers and leadership is an existential crisis that requires far-reaching, concrete solutions. This means starting at the foundation — healthcare’s outdated culture — and building again from the ground up, focusing on the mental health and wellbeing of the workforce so they can continue to provide compassionate, safe, and effective care for patients.

