This article is part of the Designing for 2035 report.
We’ve identified four dimensions where healthcare will evolve substantially by 2035, each building on underlying trends and dynamics that are evident today and that will lead to an industry that looks quite different in the future. We need to confront current limitations and constraints and be willing to embrace these evolutions if we are going to fulfill the promise of a healthcare industry that is better aligned to meet tomorrow’s needs.
Technology innovation will create step changes in processes and outcomes
Technology is getting faster, cheaper, and smarter by the day. What does this mean for healthcare? The Human Genome Project officially ended in 2003, at a cost of $2.7 billion. Today, whole genome sequencing can be done for $600.
Costs will continue to come down; the barrier now is the workforce and the actionability of data collected. By 2035, comprehensive genomic sequencing will be a standard part of medical evaluations, providing insights into an individual’s predisposition to diseases and guiding personalized treatment plans. We’ll also see advanced diagnostic capabilities propagate in the next decade: point-of-care devices and at-home testing kits will provide quick and accurate results for a wide range of medical conditions, enabling early detection and timely treatment. Additionally, pharmaceutical companies will use predictive models to design and test potential drugs in a matter of days or weeks, rather than the years it currently takes. The telehealth models of 2035 will evolve to seamlessly integrate advanced artificial intelligence, remote diagnostics, and virtual reality to provide a comprehensive, personalized experience for patients as they shift from virtual to in-person care.
Technology is necessary but not sufficient. It is the focus of this section, but true impact will require operational changes. Below are five ways that a combination of technology and operational improvements will alter the healthcare landscape by 2035.
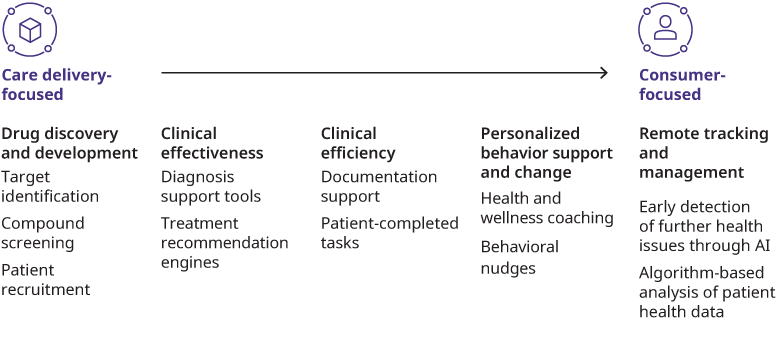
Improving processes across the care continuum
We are able to capture and analyze larger amounts of patient demographic data across more patients, allowing us to develop more equitable clinical pathways. The overall increase in information on outcomes and practice patterns, along with more effective dissemination of data, will lead to a healthcare system that is more readily able to learn from itself. Additionally, clinical evidence that is seamlessly integrated into electronic health record systems will foster faster and more accurate treatment decisions. Today’s struggles with interoperability will be overcome, and data will follow the patient in a more efficient manner. Doing a better job of incorporating data into clinical workflows will help ease the burden and burnout that clinicians currently feel from cumbersome technology systems.
Extending the reach of care processes through connected technology
RPM will stand for remote patient management, not just monitoring. Today, healthcare produces roughly 30% of the world’s data. Advances like embedding diagnostic tools into smartwatches or generally making them more compact, expanding biomarker testing, and more will enrich the quality of this data. By 2035, we’ll be able to handle this data much better. Adjacent advances in computing power will process disparate sources for a more comprehensive and accurate picture of the patient. Automated analyses systems, built on top of the infrastructure, will act as a first line of defense, triaging input data, suggesting interventions based on patient needs, and escalating care as needed.
Aiding in identifying and developing new therapies
Two key levers in the research and development process will see big advances — drug discovery and clinical trial design. Advanced computational methods will analyze vast biological data sets to identify novel drug targets with higher accuracy, and technology driven advancements in high-throughput screening techniques will expedite compound screening processes. Technology advances will also be used to identify and recruit suitable clinical trial participants more efficiently, matching patients with trials based on their profiles, accelerating recruitment, and improving trial timelines. We could also see institutions beyond academic medical centers running clinical trials, expanding access to a larger patient population. Together they will help address the gender and racial diversity gaps that currently exist in clinical trials. We can also simulate trial participants using technology, lowering the time and cost it takes to get a drug to market. The Unlearn digital twins is an early example. This technology allows a control arm to exist when one would otherwise not be possible, greatly speeding up the time of these trials. Finally, better real-time monitoring of patient safety and data quality during clinical trials will reduce errors and overall improve outcomes.
Scaling personalization of health behavior guidance in real time
Tailored programs like health and wellness coaching or behavioral nudges will become ubiquitous in everyday life. Virtual assistants and mobile apps will provide individuals with real-time guidance and support tailored to their specific health goals and needs. These will rely on generative artifical intelligence (AI) and large language models to build more personalized ways of collecting patient information and engaging with patients to get behavior change, and leverage data from wearables and health records to optimize outcomes.
Elevating labor productivity for greater focus on value-added clinical tasks
We have already seen some advances in technology providing administrative support. Further improvements will largely be in the vein of modifying ChatGPT-like solutions for creating more efficiencies of back office and other administrative functions.
Additionally, AI will support and evolve work completed by nurses, case managers, and social workers. Smart implementation of AI systems has the potential to automate some tasks completely, including prior authorizations, care planning, and consultations triggered by assessments. One net new automation that may develop is robotic medication administration which can identify routine drugs that best serve select patients. While these advances will significantly improve everyday efficiency, the rate of adoption will be limited by cost and resource shortages. Once we reduce this barrier, hospital systems can implement fully baked solutions to optimize operations.
Improvements in interoperability will lead to more advanced marketplaces and better user experiences. With this, we’ll see the continued rise of more portable and effective health records and advances in consumer-facing applications such as scheduling. Additionally, better privacy and application programming interfaces will emerge to capture, store, and share data.
Advances in therapeutics will change care pathways
We have moved past developing small molecules and running them against disease models to see what sticks. Our understanding of human biology is deepening, from how genetics are expressed in vivo to the impact of exogenous forces on disease progression. The number of drugs continue to increase, and the quality, as measured by ability to modify or even cure disease, will also improve.
New Curative Drugs
This first category includes therapies affecting diseases that were previously debilitating and often considered a death sentence. Innovations like cell and gene therapy not only offer effective long-term treatment but offer the promise of a cure. One example is CAR-T cell therapy for hematologic diseases like acute lymphoblastic leukemia. While additional care and monitoring may be necessary, the progression of the disease itself is halted. Treatments will be complex and require specialized sites of care — very few of which exist today. Another challenge standing in the way of this bucket is their high prices — Hemgenix for hemophilia B costs $3.5 million for a single treatment, creating funding and access issues. To partially combat these access issues, we’ll see the emergence of high-risk pools and more portable payment models. Current indications for this technology are in the rare disease space but it’s possible to envision more and more prevalent conditions — therapies for sickle cell and Parkinson’s disease are on the horizon within the next five years.
Drugs That Enhance Continuum Of Care
The second category of innovation is improved therapeutics coupled with advanced diagnostics to better manage conditions and optimize outcomes. The main vectors for change are more specialized drugs and better diagnostics that aid in patient matching. Examples of conditions that would benefit from this include type 1 diabetes and multiple sclerosis. Patients typically cycle through multiple therapies over the course of their journey with these diseases or stay on the same expensive therapy for 10-plus years. Projected advances in diagnostic technology, like the ones outlined in the previous chapter, will help identify the right drug for the right patient at the right time. To optimize treatment, providers must work with patients to identify the correct patient-drug combinations, and step-therapy workflows must be changed so patients don’t have to experiment with therapies that aren’t best for them in the long run. This will all result in fewer treatment cycles, leading to lower total costs, an improved patient experience, and increased adherence.
Drugs That Improve Chronic Management
Chronic conditions affect nearly 60% of adult Americans. Improving overall population health by solving these conditions will have massive implications. Consider the attention to obesity, which is a precursor to chronic metabolic diseases, not to mention the other long term downsides. Used in combination with lifestyle management, GLP-1s offer a solution for obesity that reduces the reliance on invasive interventions and multiple medication regimens. While these therapies are the cheapest of the three categories at the per-patient level, they are still expensive and the overall budget impact will be enormous. For providers, these medications may offer a more effective and tailored approach with lower risks for the patient. For payers, the bet is that treating these conditions in the near term will lessen the chance of an expensive health event in the long run. We are still in the nascent days of using GLP-1s to treat obesity. It remains to be seen if they’ll become ubiquitous or if prescribing patterns will be more discerning.
Redistributing care to optimal settings
Hospitals have been important sites of care in our system for two main reasons: Economies of scale — reducing the unit cost of care delivery through asset utilization and economies of scope — and using various capabilities and expertise to bend the cost curve and respond to patient variance. But as care delivery has advanced, the impact of economies of scale and scope has diminished. Scale no longer requires being everything to everyone. Likewise, scope needs are lessened through the ability to manage risk and reliance on more precise diagnosis.
The current inpatient model has limitations: it is capital and staff intensive and therefore expensive. It is not always the safest or most consumer-friendly place to be treated. On top of that, patient preferences and logistics may make being at home the optimal site of care. In response to this, we predict care settings will shift dramatically over the next decade.
Shortening Length Of Stay
Care that begins in the hospital will be able to move to the home more quickly by 2035. This will be led by the expansion of minimally invasive procedures, more effective medication, and an increase in available remote patient management devices.
Inpatient To Outpatient
Advances in medical technology will allow care for certain conditions and surgical procedures to no longer require an inpatient admission. This shift is already underway, with eight common surgeries experiencing a disproportionate number of outpatient cases in 2020 compared to the few years prior to the pandemic. Shifts in care protocols, including minimally invasive procedures and improved rehabilitation techniques, will push this transition. Retail clinic settings will also have an impact through enhanced accessibility, cost reduction, and a stronger focus on preventive care — meeting patients where they already frequent to provide healthcare services.
Outpatient To Home
New technologies and treatments allow providers to assess a patient’s condition virtually, currently for the most common incidences. By 2035, this will increasingly happen for complex situations. For the average individual, 28% of the services they receive in a given year are feasible via virtual care. Virtual-focused innovations that allow patients to conduct physical exams themselves while supervised by their physician are an example — thermometers, otoscopes, stethoscopes, and scales that are connected to an app and send real-time information to care teams.
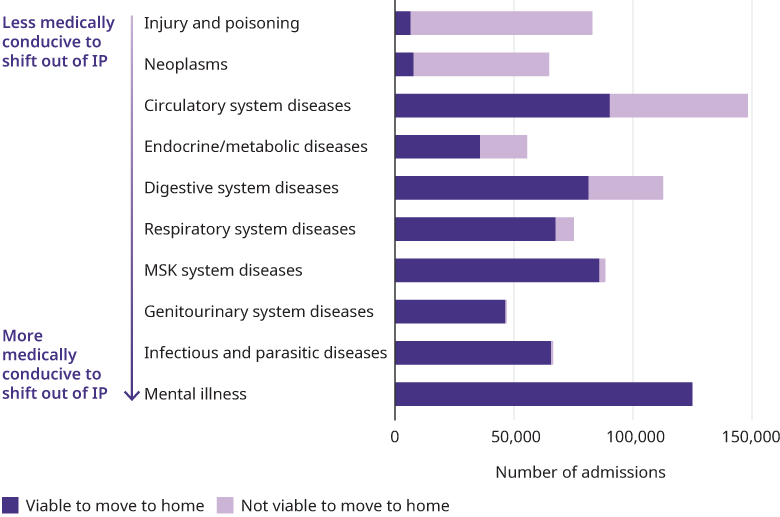
Inaptient To Home
While the shifts outlined above will all become more common over the next decade, the most disruptive transition will be from inpatient care to care at home. We project that 64% of inpatient admissions would be available to occur at home by 2035. This will be enabled by both improved therapeutics and more effective virtual care. There are several drivers that will propel this transition:
Reimbursement pressures: At-home care will be largely cheaper than inpatient care. With continued pressure on fee-for-service economics and government lines of business — Medicare and Medicaid — being largely unprofitable for hospitals, these cost savings will be embraced by most stakeholders.
Aging population: Inpatient utilization is expected to increase as baby boomers age. Building off the discussion in chapter one, the average Medicare admission is roughly four times as long as the average commercial admission. This increased demand is not met with an increasing supply of hospital beds, so innovation outside of the traditional inpatient system will have to occur to help supply meet demand.
Better technology: The Internet of Things allows for more effective at-home care where patients can immediately connect with their provider via video, phone, email, or text and upload real-time information to their medical record. This convenience also saves patients in travel time and cost and allows creates efficiencies for providers.
Patient preferences and satisfaction: Studies show that hospital-at-home patients are four times more likely than acute care inpatients to be satisfied with their physician, six times more likely to be satisfied with the convenience of care, and three times more likely to be satisfied with the overall experience. These numbers will rise as technology facilitates an even better experience.
Better outcomes: A recent study shows that hospital readmission rates were lower for hospital-at-home patients compared to hospital inpatients (8.6% vs. 15.6%). This, coupled with the fact that many complications inpatients experience can be lessened at home — lower rates of delirium (9% vs. 24%), bowel complications (9% vs. 16%), and emergency situations (6% vs. 11%) for hospital-at-home patients — reinforces the argument for migrating more care to the home.
Equity benefits: At home care programs also serve to bolster efforts that address social determinants of health. Giving clinicians and care teams more direct access to the home, especially in low-income settings, enables them to get a broader view of environmental impacts on someone’s health.
Still, at-home care has limitations. Shifting out of an inpatient setting is not feasible for highrisk situations or overly invasive procedures. And to be clear, not everything that is available to move to the home should. The overall infrastructure still isn’t robust enough to match the potential transition. Only 10% of US housing stock is aging-ready currently, and large swaths of rural America, as well as some inner cities, still lack access to broadband. For any of the above to play out at scale, issues like those must be tackled. This uncertainty is playing out in the market, where two major health systems recently stopped offering hospital-at home programs.
Health insurance will evolve significantly for certain benefits currently on the fringe
As the healthcare landscape changes, payers must modify their products to meet evolving consumer demands. While the core medical benefit will remain similar barring significant regulatory action, we will see more mental health coverage and a new approach to pharmacy coverage — each benefitting from a higher percentage of the total benefit spend and more personalization within products.
Mental health benefits will be on par with medical and surgical benefits, as required by law. Access to these benefits will increase through the use of technology in both the form of better patient-provider matching and artificial intelligence-powered bots. Coverage for non-clinical behavioral health solutions like peer support services and subscription-based apps will be the norm.
Pharmacy benefits management will be integrated with medical, not separate as it is today. For high-cost, curative therapies, financing will be pulled out into high-risk pools that follow patients. Value-based pricing will be the norm, with pharmaceutical companies taking risk not just on drug spend but also medical spend.
Products in general will be increasingly consumer-driven and personalized as well. This extends past traditional point solutions or advocacy. The market in 2035 will have tailored benefits products that enable individuals to spend their out-of-pocket dollars in areas that will most benefit their health. At the less extreme end, this may take shape as an HMO or POS plan. At the more extreme end, plans that auto-adjust benefits based on health history will emerge. Individual lines of business will experience their own evolutions, on top of the industry-wide changes.
Commercial and Affordable Care Act — division among smaller and larger employers
Group insurance trends will vary by market and will depend on the strength of local economies, local regulation, and employer attitudes toward benefits. Places with high unionization, regulation of benefit levels, and significant industry concentration may continue to see competitive, richer benefits, while right-to-work states with less industry concentration will see benefits taper off. Because of this, we project an employer market that roughly resembles what we have today. However, a few things could meaningfully shift the group insurance market by 2035.
A growing number of employers are turning to individual coverage health reimbursement arrangements to meet the ACA’s employer mandate. Through ICHRAs, employees are reimbursed for some or all the premiums of an individual plan they purchase on their own. Since launching in 2020, ICHRAs have grown by 350%, according to the HRA Council. There was 171% growth between 2022 and 2023. If we see acceleration of ICHRAs, more consumers will end up on ACA plans. With that, we expect tighter networks and benefit designs. Similarly, state governments are likely to continue pushing the envelope with public options. Colorado, Nevada, and Washington have gone down this road.
The need by large employers to enrich benefits offerings will force greater scrutiny of return on investment for what each benefit contains. Point solutions of today will be seen as table stakes in 2035. Overall point solution fatigue and a need for customization will lead to the growth of aggregators. In parallel, employers will align their benefits to maximize the return on investment on the solutions they deploy.
Currently, many small employers self-fund to avoid facing premium taxes — the percentage of small firms offering self-funded insurance rose from 13% in 1999 to 21% in 2021, a 62% increase. If regulation to close this loophole emerges, this percentage will decrease.
When we look at the ACA market, products will emerge that are designed to better anticipate evolving member needs. A greater push for standardization should eliminate the current problem of too much choice, and narrower bands of actuarial values and increased transparency will allow consumers to more easily compare products.
Medicare — Increased margin pressure
For Medicare Advantage, the Centers for Medicare and Medicaid Services will look to tweak the existing infrastructure to lower costs, by moving goalposts in the Stars Ratings program, increasing clawbacks, and making changes to risk coding. Smaller plans will fail to adapt, driving 90% of plans currently operating to close. Medicare Advantage as a whole, however, will continue to grow — with penetration up to 70% from 48% today. Traditional Medicare will continue to see a growth of alternative payment models to try and derive better value. For both, there will be greater focus on equity and stricter guidelines around access.
Medicaid — A story of integration
Despite ongoing pressure on state finances, the shift in Medicaid reimbursement policies will create opportunities for private capital investments. The venture capital market will play a larger role in Medicaid innovation over the next 10-15 years. With rising enrollment, increasing healthcare costs, and stricter budgets, states will need to find new ways to deliver care while maintaining costs. States will expect plans to offer an integrated offering across Medicaid and ACA — something that is happening in Rhode Island. Elsewhere, we are seeing insurers that already participate in the ACA and Medicaid venture deeper into this integration by transitioning people who lost Medicaid coverage due to redetermination into an ACA plan. There will also be greater emphasis on the integration of care that has historically been at the fringes, including dental, where over half of states only cover emergency services, and behavioral health.
For dual eligibles, there will be a shift away from coordination-only special needs plans to fully-integrated dual eligible SNPs. Already, 22 states have fully or partially integrated care models. The market will increasingly demand Medicaid plans tailored to high acuity patients and to lower acuity patients, resulting in necessary and bifurcated businesses.
These four major pieces of the healthcare puzzle in 2035 will greatly influence the speed and scope of healthcare’s evolution over the next decade. With ever-evolving technology impacting a wide array of healthcare processes and sites of care, continual advances in therapeutics changing how we treat conditions across the spectrum, and the healthcare product market needing to modernize to keep up, the industry of 2035 will look different across the board.

