Editor's Note: For more information, read the full report – The Digital Frontier of Health Promotion and Prevention – by Oliver Wyman, written with input from the Singapore Health Promotion Board.
Since the advent of the novel coronavirus disease (COVID-19), people’s general healthcare, health, and wellness behaviors have changed drastically. In the meantime, people are living longer. Global average life expectancy, for example, has increased by 5.5 years to age 72 over the past two decades – the fastest increase since the 1960s. Despite this significant progress, health risks remain as a health and wellness “pandemic” continues: a rise of non-communicable diseases (NCDs) such as cardiovascular disease and cancer and their corresponding health risk factors. NCDs account for 70 percent of global deaths, or 41 million people. But there has been slow and inadequate progress in addressing existing gaps in NCD prevention. In short, there was a health pandemic before a health pandemic.
Health promotion is more important than ever
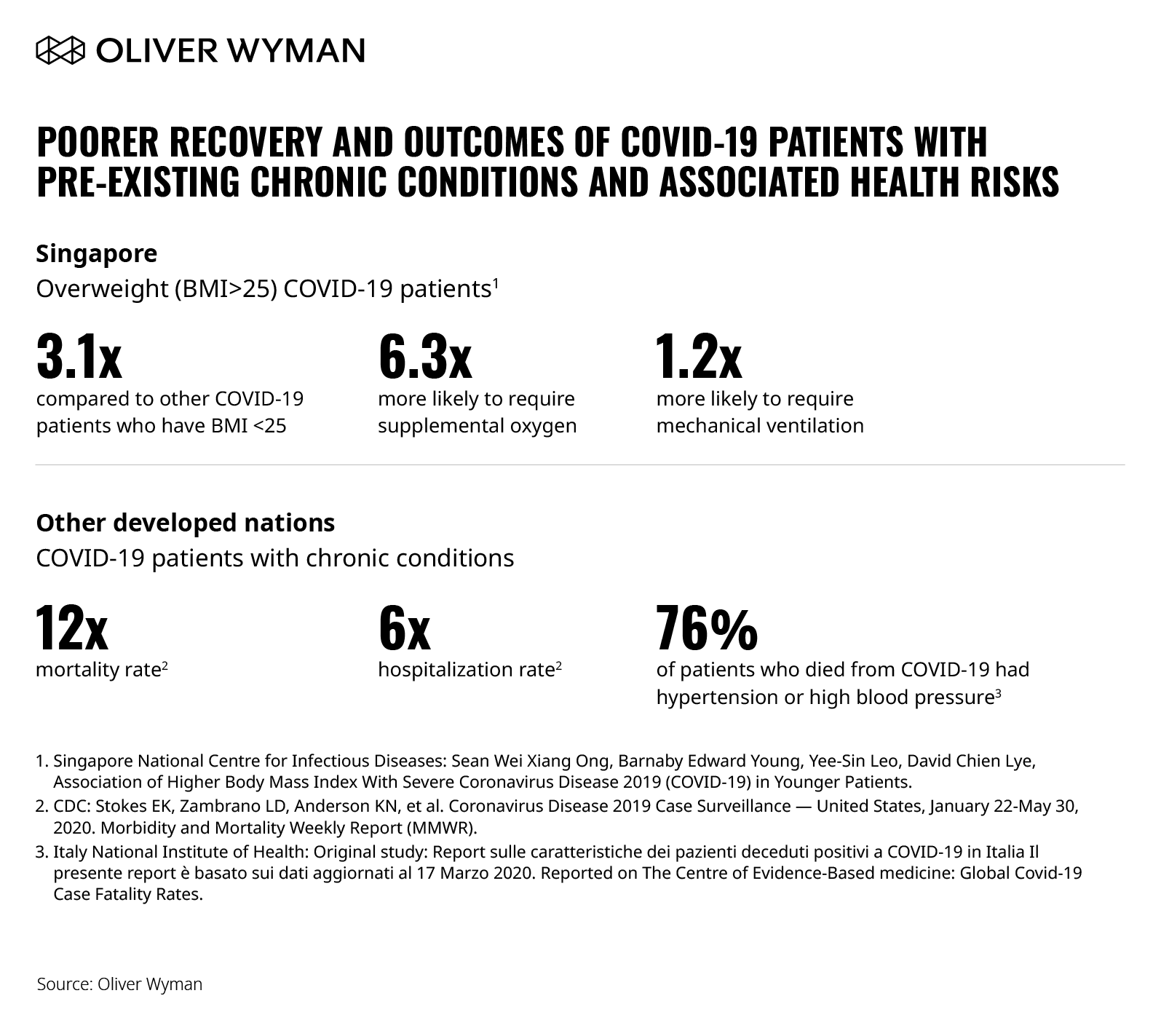
Disease prevention and health promotion have been at the core of fighting COVID-19. Beyond containing the virus, there’s a critical need for a healthy and well baseline population, amplifying the importance of health promotion and prevention. Individuals with NCDs and health risk factors like obesity are more vulnerable with COVID-19. The impact of NCDs and COVID-19 is two-fold: individuals with NCDs are more susceptible to becoming severely ill. They also have poorer recovery with COVID-19. As Figure 1 below shows, many studies have demonstrated similar evidence – both in Asia and globally.
Globally, healthcare has predominantly focused on “sick care,” rather than health promotion and prevention. COVID-19 is changing the narrative. Health promotion is even more important now – to combat COVID-19 and to better respond and support the growing NCD “pandemic.” As important as the fight against COVID-19 is, the continued support to positively influence the behavior of individuals to promote a healthy life is essential – including supporting individuals susceptible to NCDs or management for those with existing NCDs. Individuals will continue to face growing and greater health risk factors and NCDs, affecting their health and wellness. The continued investment in health promotion and prevention (including screening, treatment and NCD management) must be reinforced to support and manage the increased risk.
Changed health behaviors have and will continue to impact “well-care”
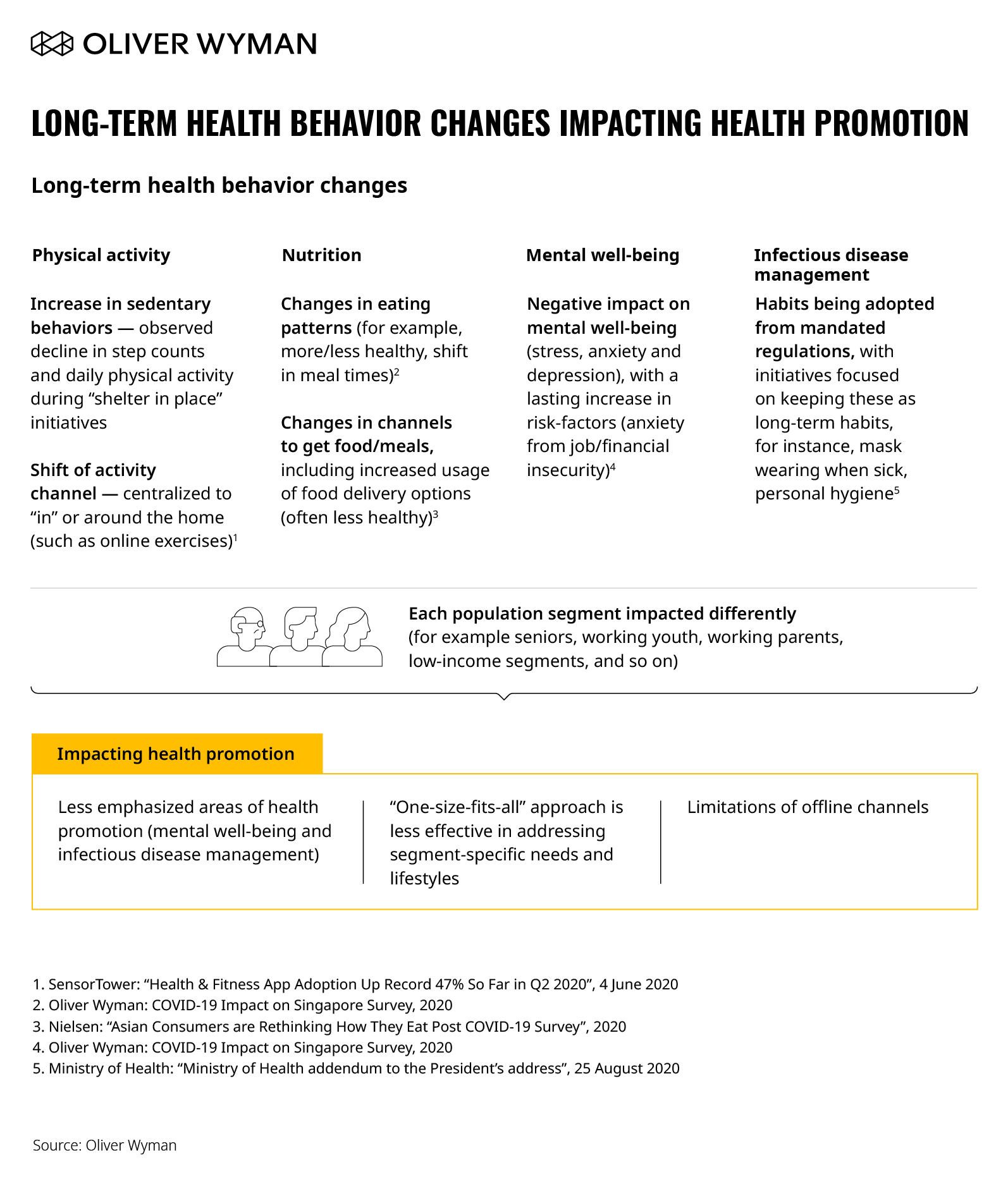
As COVID-19 spread across the globe, many public authorities responded by recommending or introducing a variety of measures to curb virus spread. Some restrictions and new ways of living are here to stay, whether driven by long-term pandemic suppression efforts or adapted consumer behaviors. For example, work-from-home continues to be the default arrangement for many and is likely here for the long-term, with some companies already declaring support for working from home indefinitely (for example, Twitter and Square). This new arrangement will change health behaviors – whether it is less physical activity, more meals consumed at home, or shifting levels of mental wellbeing tied to working from home for prolonged periods. In Figure 2, we describe the new health behaviors here to stay across four health promotion domains. These behavioral changes expose and highlight key gaps and challenges faced in health promotion moving forward, namely:
1. Unmet needs in less emphasized areas of health (like mental wellbeing and infectious disease management).
2. A “one-size-fits-all” approach is less effective in addressing segment-specific needs and lifestyles.
3. There are limitations of offline channels for citizen reach and engagement.
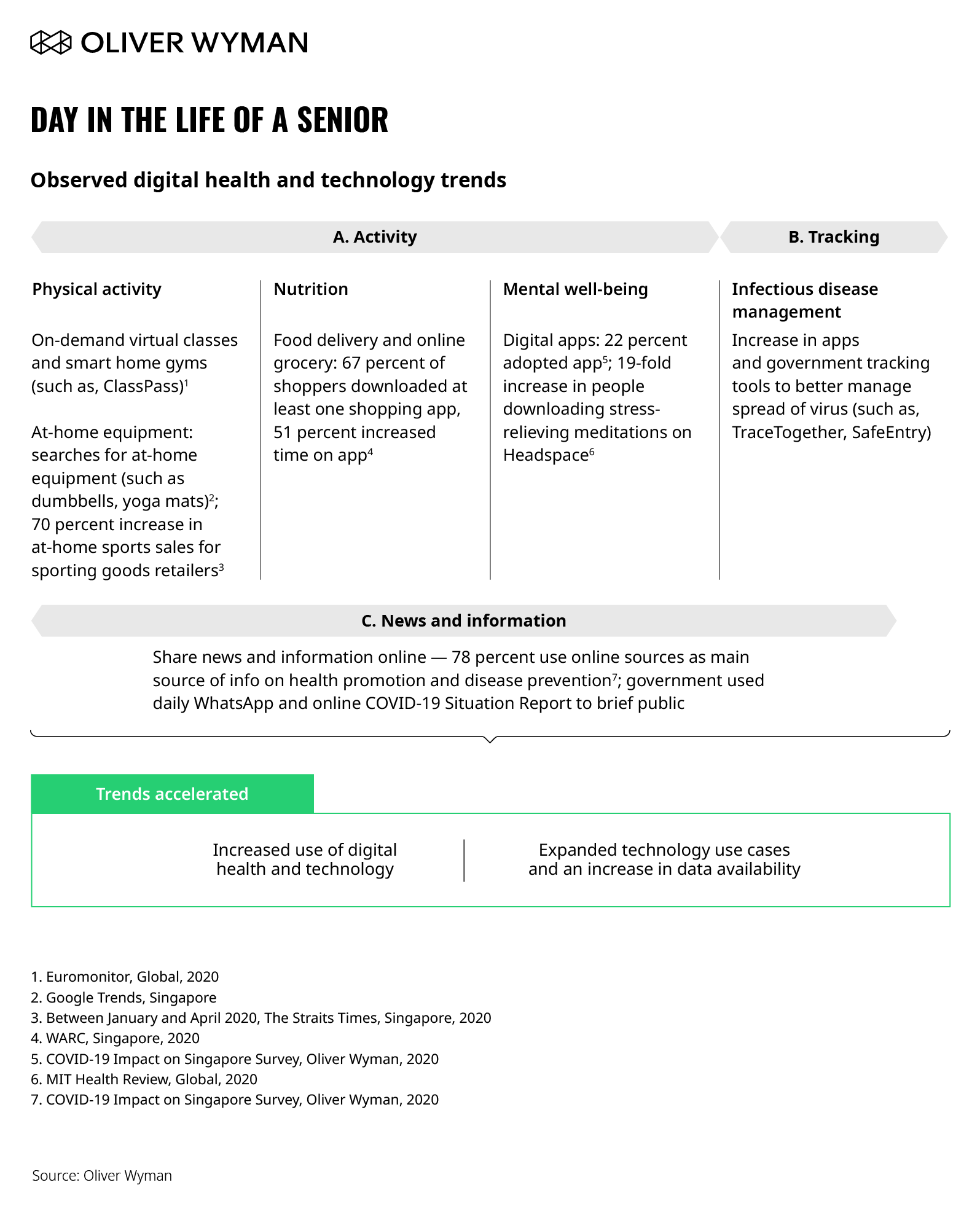
COVID-19 has accelerated technology and digital adoption. There has been an increased use of digital health and technology across citizens and private and public sector. For example, consider that the global smartwatch industry observed a 20 percent growth in the first half 2020. Technology has also rapidly expanded use cases, from COVID-19 detection to new digital health initiatives (for example, LumiHealth – a first-of-its-kind personalized digital health program developed by the Health Promotion Board and Apple).
Reimagining the way forward in a post-COVID-19 world
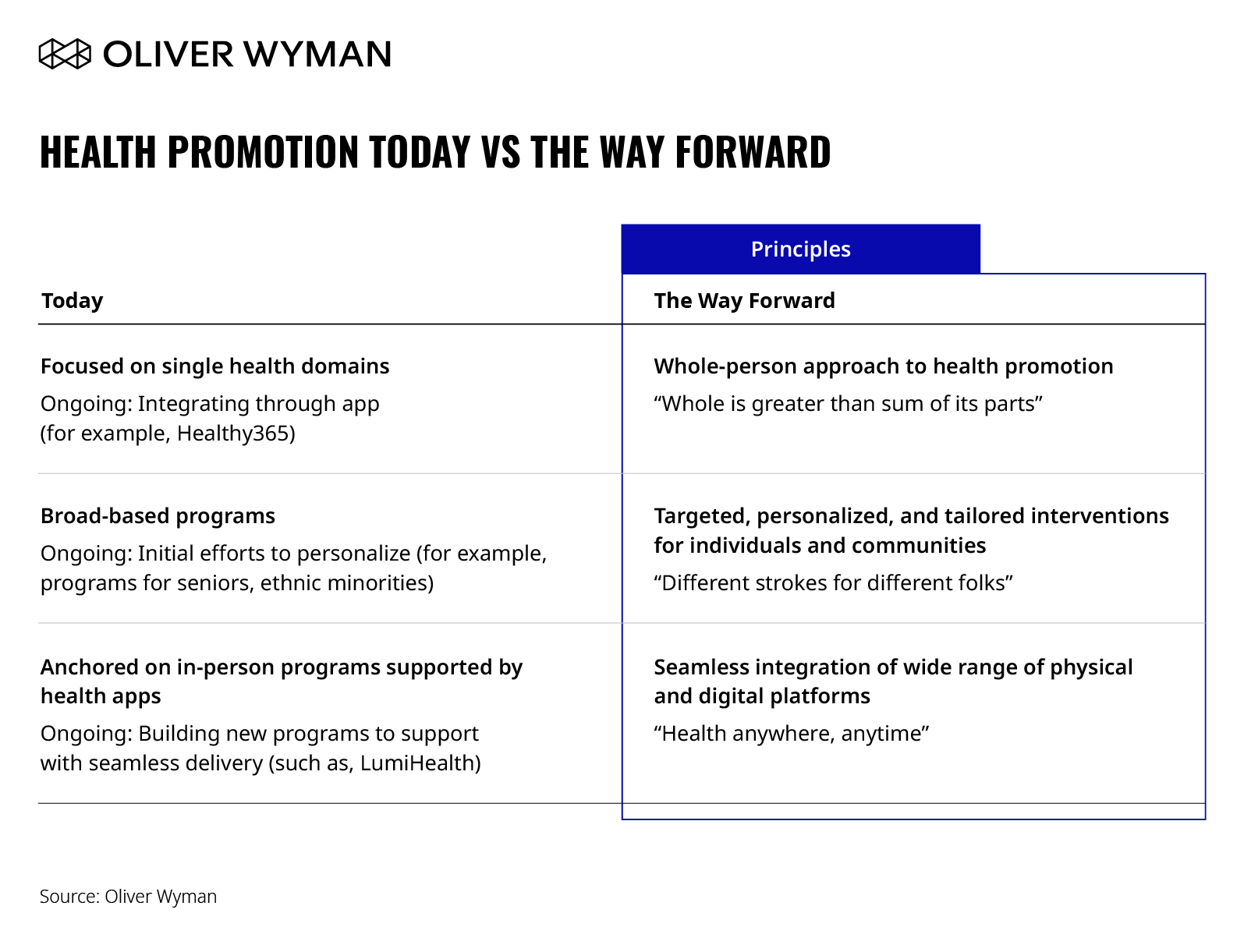
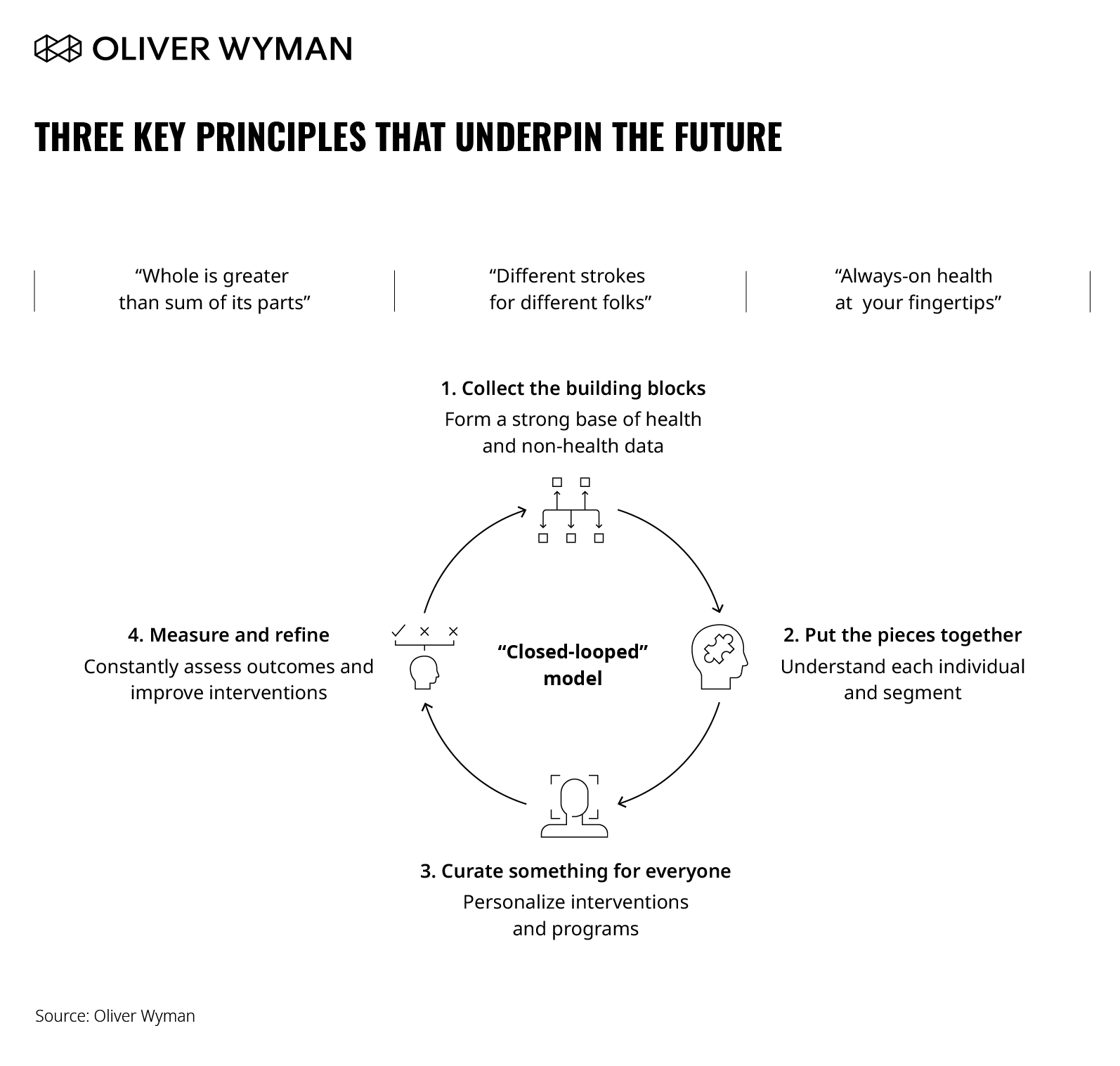
With good momentum of digital engagement coupled with a renewed need to focus on health promotion, now is an opportune time to rethink health promotion and the role of data and technology. Based on the challenges and digital health and technology trends observed during COVID-19, we define three key principles that underpin the future of health promotion.
These three key principles necessitate a “closed loop” model for health promotion. The “closed loop” is a framework to support any organizations in designing and implementing evidence-based and effective interventions and programmes that improve the physical and mental health of a population. The model should distil key information from individuals (such as health habits and preferences) into targeted and personalized interventions, continuously improving and evolving based on further inputs and outcomes – ultimately creating a “closed loop” model of health promotion.
1. Collect the building blocks
The first step is to build a foundation of data. A comprehensive and accurate dataset is crucial to forming a fact-based view of the individual and the population. Connected devices such as smartphones and wearables can enable an ongoing “autopilot” of data collection across a range of health data. Other sources of information such as electronic medical records, disease registries, or even supermarket purchases can further contribute. Data collected is not only real-time but is also longitudinal and cross-cutting (for example, tied to a specific person across metrics). This enables insights to be increasingly precise and predictive. Equally as important is building public confidence on data privacy as data collected will only come if individuals allow it.
2. Put the pieces together
Combine and analyze data to better understand the individual through health needs and risks, habits, and behaviors. Drawing links between different types of data can define more granular population segments beyond traditional filters such as age or gender. For example, a comprehensive health risk score can be developed based on a combination of health factors and identify “high-risk” individuals. Further, as analytics tools continue to become more powerful, analysis will shift from descriptive and retroactive to predictive, allowing for segmentation to be increasingly more granular and precise.
3. Curate something for everyone
With an understanding of needs and habits, evidence-based interventions can be developed and tailored. This will translate to individuals having the flexibility of accessing healthy lifestyle interventions and options beyond traditional channels, drastically increasing the ease of access and frequency of touchpoints. Better granularity will also enable activating specific communities around key health issues.
4. Measure and refine
The final step of the “closed loop” model is arguably the most important. At the core of the model is improving health outcomes of the individual which means measurement is imperative. The interventions must be assessed against measurable and consistent benchmarks. By evaluating the outcomes of the interventions, health promoters can better understand what works and what doesn’t and recalibrate accordingly.
These findings and results create yet another source of data, further growing the base of data and information available for analysis and development of interventions – thereby closing the loop and creating a virtuous cycle of health promotion.
What are the implications for different health system stakeholders?
Health promotion and public health authorities will become even more front and center as there is an even stronger need for deeper and smarter investment of resources into health promotion, including building the “closed loop” model.
Healthcare systems also have a part to play in the transformation as a key patient touchpoint for data collection and patient interventions. They also stand to gain from bending the cost curve and reducing preventable admissions through more effective health promotion and disease prevention measures.
Private sector players are presented an opportunity to scale through partnerships with the public sector. While they often have best-in-class technology solutions in digital health, they may not have the requisite public health knowledge, strategies, policies, and reach to expand beyond their existing user base or have access to a larger population to deploy their technologies or solutions. The private sector can also benefit from strengthening their brand by meeting public needs and improving health education and conditions worldwide.