Editor’s Note: The following article is an edited version of a conversation that originally appeared on the Oliver Wyman Health Podcast and the Oliver Wyman Health Innovation Journal, Volume 4.
The idea of healthcare services shifting from traditional, in-person delivery at clinics and hospitals to digital delivery at home is not new. That value proposition has been obvious for years: For the more than 7,000,000 people who are housebound or have mobility limitations, home care means accessible care; and for the two-thirds of emergency room visits that are avoidable and that cost the healthcare system $32 billion each year, home care represents a meaningful opportunity to deliver higher value, lower-cost care. Surveys repeatedly show consumers prefer home and digital care services. This is because these services feel much more personal, and the contextually rich environment they’re delivered in can improve outcomes.
For decades, home care has focused on delivering high-acuity, labor-intensive services such as caregiving for the elderly, conducting health assessments, doing infusions, or providing palliative care. More recently, we’ve seen this focus expand – in response to consumer demand, accessibility issues, and economic pressures. Home and digital hubs are being considered for nearly the entire spectrum of healthcare services – from low-acuity assessments and primary-care physician visits, to highly intensive programs such as Hospital at Home. Favorable trends in supply economics – such as technology-enabled care, changing reimbursement regulations, market diversification, and the consolidation of home health agencies – have been positive tailwinds. Most of us anticipated the shift to home and digital care to be gradual…and then the COVID-19 pandemic struck. Telemedicine rates have skyrocketed over 100 percent month-over-month at many provider systems. The home is the de facto preference for most consumers seeking healthcare today. Will these trends sustain? And, who will “own the home”?
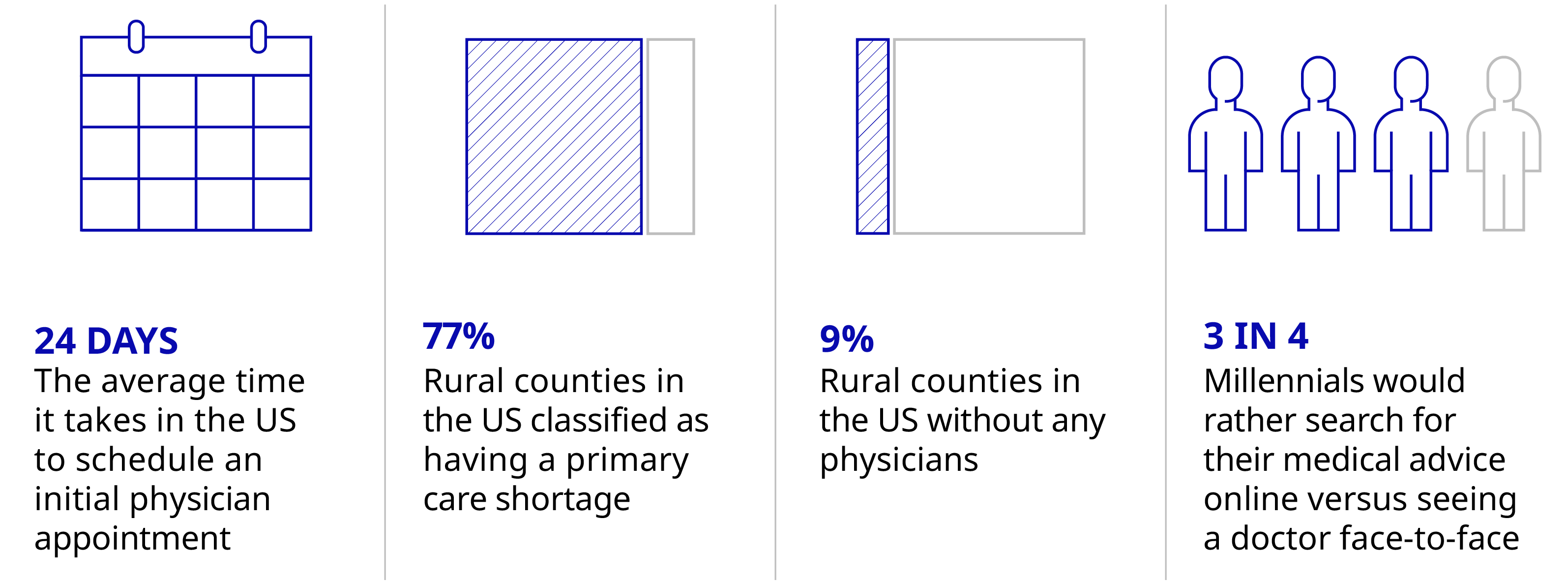
Setting the Scene: Four Telehealth Stats to Know
Source: Merritt Hawkins: 2017 Survey of Physician Appointment Wait Times and Medicare and Medicaid Acceptance Rate, National Rural Health Association, RuralHealthWeb.org, Harmony Healthcare IT, Survey Reveals Millennials’ Relationship with Health Care, August 2019
Q&A with Omada’s Sean Duffy and Physera’s Dan Rubenstein
To discuss the seismic shifts in care delivery models, Oliver Wyman’s Adi Lingampally, sat down with Sean Duffy, CEO and co-founder of Omada Health, and Dan Rubenstein, CEO and co-founder of Physera. What follows are highlights from their conversation.
Adi: Let's start by discussing some recently announced healthcare news: Teladoc announced its acquisition of Livongo for more than $18 billion. What are your thoughts on that deal?
Sean: It’s a massive validation for a virtual approach to health. It's a statement of the times that the deal of healthcare everyone's talking about this year is a deal involving digital care. At Omada, the motto/mantra we've long held is that in-person healthcare is option B. We are thinking about ways to increase value, affordability, and experience by delivering services from afar. This merger is a huge validation of that. It is where healthcare is going.
Ahead of COVID-19, I thought it would be a 10- or 15-year journey to get there. In March, basically overnight, hundreds of millions of Americans started to ask themselves, “Can I get care without having to show up in a doctor's office or without having to sit in a waiting room?” And if you think of the dominoes it triggers, these individuals are asking their health plans and/or their employers, “What offerings do you have that can support this need?” COVID-19 is tragic in so many ways. We can all hope we end up with a better healthcare system because of it.
Adi: Dan, what kind of uptick did you see in your programs as a result of the pandemic?
Dan: We saw a tremendous uptick in interest in Physera and our offering. We had a huge increase in appointments with our providers. It's very hard for us to decouple organic growth, simply because we're growing very fast and adding new customers every quarter from growth due to COVID-19. Since the second quarter of 2020, there's been a step-function increase in our business – even when taking into account existing customers.
Our program is completely virtual. We had a number of health plans that we had been courting for months – if not years – all of a sudden calling us, asking to meet next Tuesday. It was a huge acceleration – both from the patient and the customer side – for our company. It's borne out to be a better way of doing care as a frontline treatment. You don't need to go in person, with concerns about exposing yourself to COVID-19. Having the ability to access care from the comfort of your home and getting expert advice from a specialist is valuable for people. They really appreciate having that.
We had a number of health plans that we had been courting for months – if not years – all of a sudden calling us, asking to meet next Tuesday.
Adi: How much of this growth do you think is tied to a point in time versus it being an actual transformation that's here to stay? Will this uptick in usage of digital health services be sustained post-COVID-19?
Dan: When you look at an industry like telecommunications, for example, certain countries in the world didn't have landlines, and they essentially skipped that whole infrastructure of landlines once mobile came out. There's no reason for them to go back and implement landlines now.
Similarly, now that we've seen the power and the capability of telehealth, it will be here to stay – even after the crisis has passed. It's not going to replace in-person care. It's going to continue to augment it. But, having it as a first-line treatment makes a lot of sense. We will see a structural shift. This crisis has made it possible for people to get comfortable around it across the ecosystem – patients, providers, and payers. We’re hopeful payers will continue to pay for it long after the crisis has passed.
Adi: What was it like building and implementing a physical therapy app?
Dan: The basic form of our app was very quick. We had an app out to the market within six to nine months from when we started. And of course, we've iterated and improved it over time. But the harder thing we're building is a nationwide network of licensed clinicians to provide care that the infrastructure needed.
Sean: These are difficult operational and technological offerings to create. They involve a blend of people, regulations, and licensure technology, across many dimensions.
Dan: On the compliance side, what we do is a lot more than just give a clinician Zoom, right? You can't just give a physical therapist Zoom, say, “Go,” and have them deliver effective care. So over the years, we have developed a compelling, deep program that leverages the technology of televideo chat. But at its core, there are things you do differently when providing telehealth than you would do in-person. This isn’t something they teach you in schools.
You can't just give a physical therapist Zoom, say, ‘Go,’ and have them deliver effective care.
Adi: What is your goal regarding your mission to continue driving the transformation of in-person care?
Dan: Our goal is not to replace in-person care. Our goal is to augment it – and by doing that, making the whole system more efficient. As a country, the US is spending so much money on healthcare. And we're not getting the best results. There's a misallocation of resources here. So, having a better front end for the patients who need that level of care will free up resources for other patients who need deeper care.
I don't see our mission as being about having to do everything digitally. That doesn't make sense. Ultimately, you will need to have both good digital care and good in-person care: Use the digital solution where it's appropriate, and have in-person available for those people who need it today. I feel like we’re building a new world.