Editor’s Note: The following article, originally published on Medium.com, is part of Oliver Wyman's ongoing series about the evolving novel coronavirus (COVID-19) pandemic.
CEO and Co-Founder of Iora Health, Rushika Fernandopulle, is a member of the Oliver Wyman Health Innovation Center's Leaders Alliance a coalition comprised of senior executives from all areas of healthcare who have committed to work collaboratively on key issues impacting consumer value and overall industry sustainability.
“Historically, pandemics have forced humans to break with the past and imagine their world anew. This one is no different. It is a portal, a gateway between one world and the next. We can choose to walk through it, dragging the carcasses of our prejudice and hatred, our avarice, our data banks and dead ideas, our dead rivers and smoky skies behind us. Or we can walk through lightly, with little luggage, ready to imagine another world. And ready to fight for it."
After two months of various flavors of “stay at home” orders across the country, we are finally seeing signs of returning to normalcy. In many states, people are returning (albeit slowly) to salons, shops, churches and restaurants and, increasingly, schools are announcing plans to reopen (though in a modified way) this fall. Many businesses have been severely hurt by the shutdowns, losing a large part of their revenue while still on the hook for most of their costs. Primary care medical practices, despite increased demand for services due to the pandemic, have been severely affected because of the dominant fee for service payment model. Most practices have seen nearly 80 percent decreases in visit volume, with a corresponding drop in revenue. The dominant coping strategies are threefold: 1) take handouts or relief, like federal Paycheck Protection Program (PPP) payments, 2) hunker down and temporarily furlough staff, and 3) wait for this all to blow over and hope to return to business as usual.
These options may be a reasonable strategy for some businesses but unfortunately, they do not provide a compelling roadmap for primary care. In order to meet the needs of our patients, adapt to today’s reality, and prepare ourselves for the future, we must make radical changes to how we deliver care, always putting our patient’s needs first. Iora Health is a national primary care group with almost 50 sites across the country. Because we serve predominantly older, sicker, and lower-income seniors, we cannot wait for the day when those patients can safely seek routine, in-practice care from their primary care team. Our patients need support managing their chronic conditions and acute issues, without having to leave their homes and put themselves at risk of COVID-19. While we remain optimistic that we will get a vaccine or treatment for the virus, experience tells us it will be more likely years and not months before this happens at sufficient scale to return to normal. Indeed it has been over 13 years since the original SARS virus was described, and 40 years since HIV. With huge efforts, we still do not yet have effective vaccines for either. Hope raises spirits, but it is not a strategy.
The pandemic is an impetus to radically transform how the delivery system serves patients. We have the opportunity to thrive. With appropriate humility for the size of the task, we would like to share our journey so far in the hopes it may be instructive for others — in primary care and in other industries affected by COVID-19 — to create a better future. We have structured our journey in three parts, inspired by Ford Motor Company Chief Executive Officer Jim Hackett’s framing of working simultaneously in three time frames: Now, Near and Far.
Now: Immediate Shift to Non-Visit Based Care
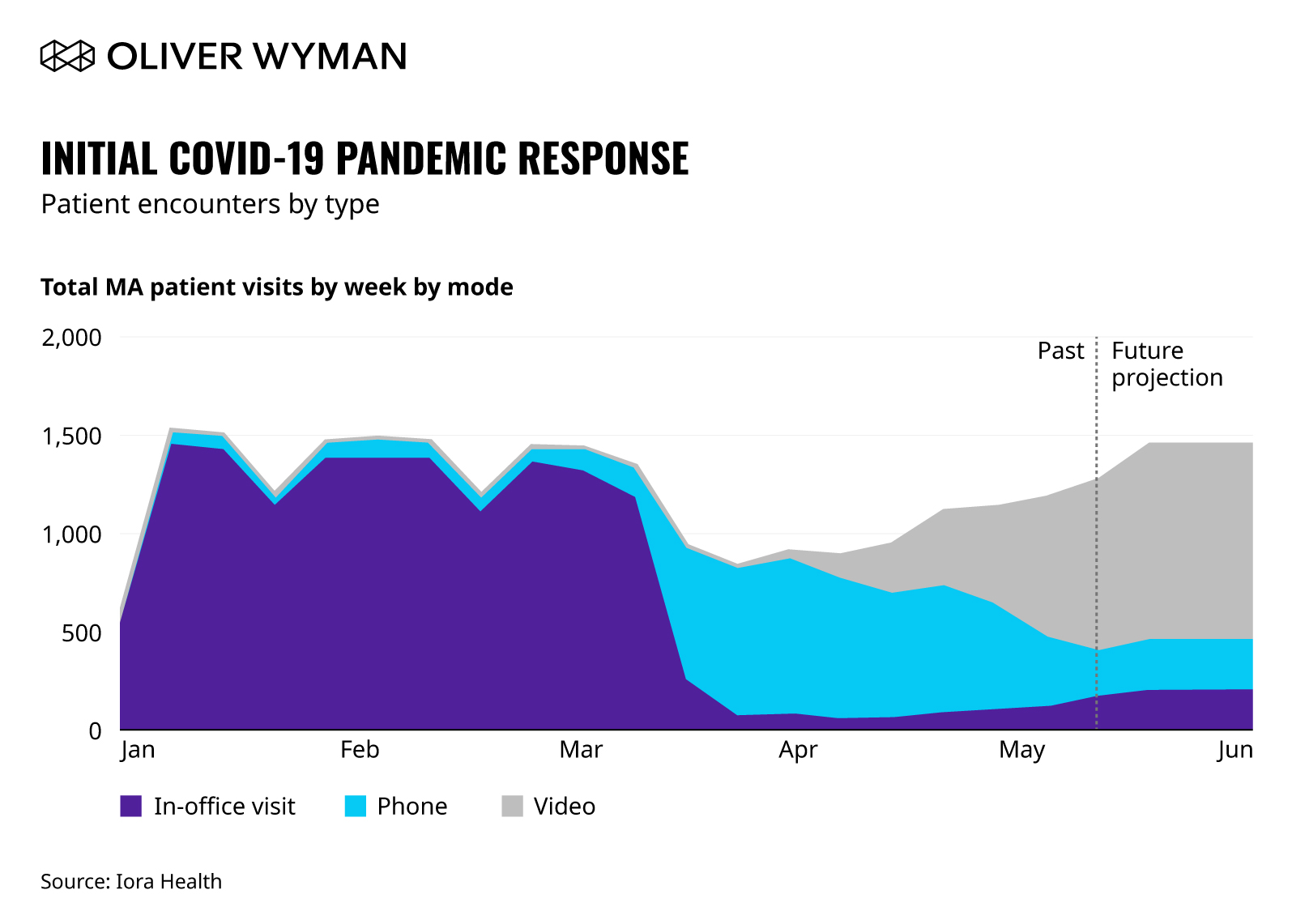
When it became clear in early March that COVID-19 was spreading significantly in the community we (along with most companies), made rapid and immediate changes in how we worked, both to protect our patients and teams and to contribute to national efforts to flatten the curve and protect our healthcare system from exceeding its capacity. We shifted literally overnight to having all our administrative staff work remotely, but did commit to keeping all our primary care practices open to see patients who needed us — but only those who required an in-person visit and only when we can conduct such a visit in a safe way for both patients and team members. Because we are not paid per visit but with population-based payment models, we have always had the opportunity to leverage non-visit based care (email, text, phone, and video) to interact with our patients; we already had the infrastructure and processes in place, so just had to turn up the dials. Within a week, only eight percent of our synchronous encounters were in-person, with the vast majority of our patient interactions happening by telephone. In addition, we committed to increasing our contact with our patients during this challenging time and doubled our number of encounters per day by proactively reaching out to check in, and make sure our patients had the food, medicines, and human contact needed to stay safe.
Initial COVID-19 Pandemic Response
Patient Encounters by Type — First Four Weeks
Patients greatly appreciated this intense outreach, especially as they saw many of their friends have trouble reaching their primary care physicians, whose offices were closed because of lack of protective equipment or staff. Said one patient, “I’m so glad you called! I was reading so much about other clinics not being available for their patients and I wasn’t sure what to do. You just made me feel so much better by calling and letting me know you are there for me and will be there for me.”
This pivot has had a profound impact. As of the middle of May, despite serving largely older, sicker, lower-income seniors our hospitalization rates and mortality rates for COVID-related illnesses have each been around one per thousand patients (not a typo — for reference typical hospitalization rates overall for Medicare patients are around 300 per thousand, and nationally hospitalization and mortality rates for vulnerable seniors have been many times what we have seen).
Near: The Transition to Video
Our first step in moving away from in-person patient encounters shifted care to telephones, as they are ubiquitous and both patients and physicians (and their teams) are familiar with their use. As we realized that remote care was likely to become the dominant way to interact with patients for the long run, we decided we had to make a second shift from phone to video. Video is superior to audio alone not only with regard to maintaining relationships, but also to detect and convey emotions and make clinical judgments and diagnoses (not just physical exam but overall assessment of how sick someone is). Because our business model is rooted in full-risk Medicare Advantage models, video encounters also allow us to submit diagnoses for hierarchical condition category (HCC) risk adjustment scores.

Iora’s Phoenix, Arizona-based Care Team Medical Director, Dr. Melissa Romero, doing a video visit with a patient. Source: Iora Health via Medium.com
Over several weeks in April, we moved from doing just a handful of video encounters to over 1,000 each week with the help of video visit champions in each market, detailed training and troubleshooting for teams and patients, and the daily use of sophisticated process improvement techniques to resolve operational challenges. We closely tracked barriers patients had with video use and developed several pilots to explore ways to overcome these. Roughly 30 percent of our patients have some barrier to using video, due to lack of appropriate devices, poor internet access, or cognitive challenges. One of the most promising strategies to overcome these barriers has been to have an Iora team member deliver a sanitized, pre-configured tablet to the patient’s doorstep minutes before the appointment and provide troubleshooting/support as needed. In the month of May, we will conduct 500 tablet delivery-enabled visits with patients who would not otherwise have the opportunity to “see” their doctor and care team. We have also shifted to Saturday hours to make it easier for our patients’ children or grandchildren to be available to help.
Access is the cornerstone of great primary care. While the onset of the pandemic reduced our ability to provide in-person care, we have responded rapidly to ensure we can interact with patients on a variety of different virtual platforms. By early June, we expect to conduct the same number of synchronous patient visits each week as we did in January and February, but with over 70 percent of those interactions conducted by video.
While not an easy change for teams or for patients, the rewards are many. Reported a formerly skeptical patient after their first video call ever (with their doctor), “From the emotional connectivity perspective, it really wasn’t different than sitting across a table from him. I think this is the best compromise in this situation — we came away with ‘That wasn’t so bad!’” We now have newly-digital patients in their eighties not just communicating with us by video, but using these skills to stay in touch with friends and family as well. And our teams are finding that in some ways video may even be better than the traditional office visits — they get a better sense of a patient’s real environment, they can include more family members including those who live elsewhere, and even finally meet their patient’s dog who they have heard so much about.
Note that this vision of telemedicine is quite different than what many think of when they describe this — a short video-chat run by a standalone company with a doctor you have never seen before (and never will again) who has no information about you helping to evaluate an acute problem. This tele-urgent care is perhaps best suited for younger, healthier people with no pre-existing medical problems and one-off complaints, but is not what older, sicker patients with chronic disease need. For our most vulnerable seniors, the ability to have an ongoing trusting relationship with a team of people (doctor, nurse, health coach, behavioral health specialist) with whom they can interact on a longitudinal basis in a variety of ways is the optimal solution.
Far: Restructuring our Teams and Process
But even this is not enough as we consider how we need to change our business to best serve our patients in the long run. Simply shifting in-person encounters to video and keeping everything else the same does not optimize care for the new COVID era. We believe the patterns of care have changed for the long term for our patients. Thinking we can simply reopen our offices and go back to crowded waiting rooms and a full schedule of office visits is simply living in denial. Our patients know this is not safe for them or for us, and now that they have experienced the ease of interacting by video, they are rightfully reluctant to have to come in person for interactions that can as well or better be done remotely.
In response to this, we have begun a comprehensive redesign of our care processes to optimize care for what we see is a long term future. This is still very much a work in progress, but we are being guided by several principles:
- Re-organize around populations and not practices. We used to think about care structured around a physical practice, and created staffing models and workflows largely around this. Now we think of small flexible teamlets — a doctor or nurse practitioner (NP), along with two health coaches building a relationship and taking responsibility for a small fixed population.
- Meet patients where they are. Instead of this team sitting in a practice and making the patients always come to them, they can interact with patients in a variety of ways, based on patient need and preference. We still feel strongly there is a role for meeting in person to build the relationship, for certain clinical encounters where laying on of hands is important, and for some serious conversations but for most other things email, text, or video can work better. When we first reacted to COVID we likely swung too far, only having eight percent of our synchronous encounters be in person. We are already at 16 percent, and think the right amount will likely settle somewhere closer to 20 to 30 percent for our population.
- Centralize the right set of services. We believe there are a set of things we do which do not depend on a direct relationship with the patient and these are best taken off the plates of our clinical teams and centralized and eventually automated as best we can. We are starting with processing faxes (it is amazing to us that in 2020 we are still getting over a half a million faxes a year!), and moving on to record requests and other such functions. Note we are not centralizing things where we think relationship matters, like requests to schedule a visit which are actually requests for care, and thus the team that knows the patient best can best respond to their needs in a flexible and appropriate way.
- Create the right sort of technology to augment care. We believe there are many workflows in primary care, such as medication management and chronic disease care, which can be helped with better technology. Note this is not what current Electronic Health Records do — they simply record care and help bill more; we need a new set of tools to optimize care. We need these to help patients and care teams improve self-efficacy, not replace it.
This work redesigning care is not easy — but it is exactly the right thing to do. This pandemic challenges us to think anew about all of our work and we need to have the courage and imagination to respond appropriately.
One of the implications of this redesign to meet the future, especially given the financial uncertainty due to COVID-19 for a venture-backed full-risk primary care group, was that we had to make the extremely difficult decision to restructure our workforce, resulting in laying off some of our incredibly valued team members. This decision was not taken lightly and was done so only after considering all of the other alternatives, but we did it in order for us to best serve our patients and not only survive, but thrive in a post-COVID world. We needed to fundamentally change our care model and how we supported it, and the way we used to do it simply no longer made sense. Pretending we could just hunker down, ride out the pandemic, and return to what we were doing before was not and is not a realistic plan. We must look forward and not backward to best balance our service to our customers (patients), teams, and our communities.
We are all faced today with leading in a world we did not expect nor wish for. This once-in-a-century pandemic is challenging all of our institutions to adapt. We can choose to hunker down, or can choose to use it to imagine a better world. This is really hard — and comes with hard choices — but the path is up to us. And we’re ready to fight for it.