Editor's Note: The following article, about our Future Truth predictions for the healthcare industry, was originally published in the Oliver Wyman Health Innovation Journal, Volume 4.
AI Will Help Us Hear Our Bodies
Here’s something you might think is science fiction but is a hard medical fact: Artificial intelligence-based (AI-based) applications can now listen to one single heartbeat and detect congestive heart failure (CHF) with 100 percent accuracy. It’s not a stretch to imagine that the dreaded nightmare of ending up in an emergency room (ER) on a gurney has now morphed into a new reality – one where you can proactively detect CHF and then walk into your doctor’s office to discuss options for managing it.
Prevention in this way is powerful. Yet, it has proved elusive for many reasons. None are more telling, perhaps, than the inability to continuously listen and harness our bodies’ voices and messages.
Preventative services constitute three percent of overall US healthcare spend. Almost 75 percent of all healthcare spend is tied to treatments for patients with chronic conditions. These figures trend even higher for publicly funded programs – as high as 83 percent for Medicaid and 96 percent for Medicare.
We expect AI will significantly enhance our ability to proactively and accurately detect the likelihood of acute events for a patient with chronic conditions and minimize expensive and unnecessary ER visits or hospital admissions. We also expect it will transform chronic care, prevention, and waste.
Seventy-five percent of healthcare spend is tied to treatments for patients with chronic conditions.
The Incoming Data Ubiquity
Access to appropriate, real-time data is crucial to enable early detection of acute events for chronic patients. Historically, this requirement has been addressed in a limited capacity through sporadic lab tests that yield results at given points of time – results that are inadequate from a prevention standpoint. For example, asthma patients who typically visit a primary-care provider every three months spend more than 2,000 hours between visits where their symptoms aren’t actively monitored. As a result, providers evaluate symptoms for a fraction (less than 0.1 percent) of the patient experience to understand and manage conditions. Moreover, electronic health records are notorious for incomplete and/or inaccurate information that is limited to provider interactions during visits.
With the ability to amass and process large data volumes through cloud computing, we’re finally at an inflection point where AI applications will bridge this gap, enabling ongoing monitoring of patients with chronic conditions. The missing component to feed AI applications – access to real-time data – will be addressed through the widespread proliferation and adoption of wearable devices. Here are three key drivers:
Ubiquitous data. Here, data goes beyond traditional medical records and claims. Access to real-time data is gathered through monitoring, wearable devices, and individual gene and behavioral profiles – the last of which is growing.
Quickly advancing computing. Computational power to train AI models has doubled every 3.4 months since 2012.
Consumer expectations. As AI applications assume a prominent role in the early detection of acute events for patients with chronic conditions, we envision a gradual shift in cost and utilization patterns. This is especially true for where and how care is delivered. For example, the National Institute of Health in the United Kingdom launched an initiative to integrate AI for the early detection of chronic conditions, with the aim to eliminate nearly 30 million unnecessary outpatient visits and save close to £1 billion over the next five years. The greater objective, along these lines, is to optimize cost and utilization and reinvest scarce clinical resources to frontline care.
Computational power to train AI models has doubled every 3.4 months since 2012.
What AI Insights Will Impact Chronic Care Management the Most?
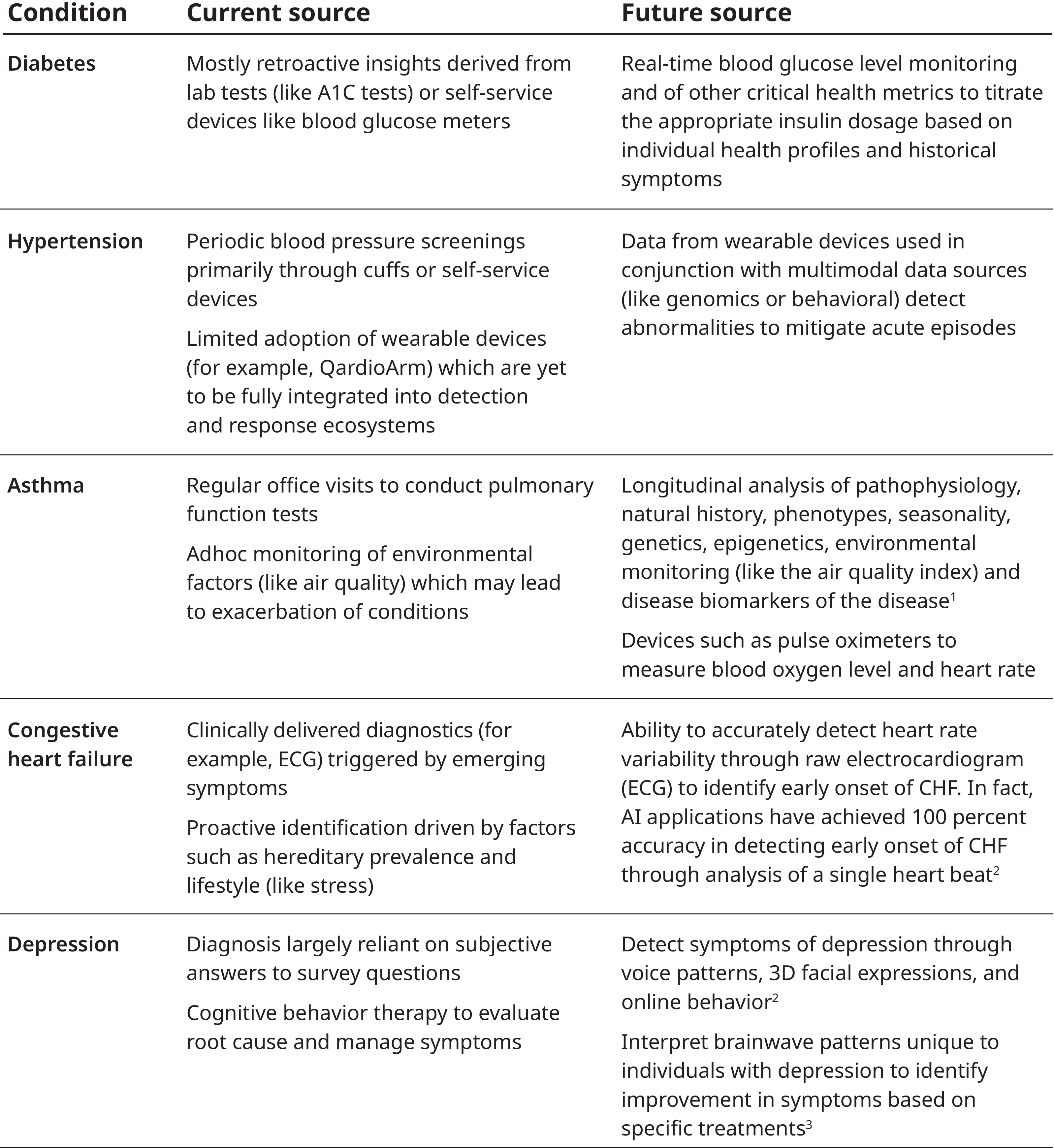
We analyzed the primary source of insights currently deployed for the detection of acute events for patients across the five most prevalent chronic conditions in the US. These include diabetes, hypertension, respiratory disorders like asthma and chronic obstructive pulmonary disease (COPD), CHF, and depression.
Sources: 1. PulmonologyAdvisor, Severe Asthma: Harnessing Biomarkers to Power Treatment Effectiveness; 2. ScienceDaily: AI neural network detects heart failure from single heartbeat; 3. MIT Technology Review: Our smartphone’s AI algorithms could tell if you are depressed | Headway, Ginger Website: Why We Created the First AI-based Behavioral Healthcare System
Early Detection Will Reduce ER and Hospital Utilization
As a result of the above shift, significant cost savings will be generated. Recent studies, for example, estimate this opportunity tops $8 billion annually.
To affect this transformation, we expect to see an evolution of business models across all major stakeholders in the healthcare ecosystem. Regardless of who the stakeholder is, the ability to ingest different types of datum while managing the data’s privacy and security will become table stakes.
The evolution of existing business models to integrate and deploy AI insights meaningfully will determine how effectively we pivot to prevention from treatment to manage chronic conditions.
This advent of powerful AI-driven insights and preventative opportunity isn’t just incremental. As an addition to the toolkit clinicians have used to understand patients and their conditions, it also will enable entirely new processes and businesses that have the potential to disrupt and drive new industry value.
Five Predictions Regarding AI’s Healthcare Impact
1. Providers will be at the forefront of deploying AI capabilities to drive the pivot to preventative care for chronic care management. We expect significant innovation in this space. AI service providers will disrupt traditional business models focused on an incremental approach for care model-design improvement.
Integrating AI application within patient and provider workflows will become critical as AI takes on an increasingly active role in monitoring, evaluating, and diagnosing chronic conditions and providers concentrate on care planning and treatment.
ER utilization will be restructured to focus almost entirely on acute care and trauma victims, as AI-based applications minimize frequent and unwarranted ER visits. We expect a dramatic shift from exacerbation-related inpatient admission for patients with chronic conditions. As evaluation and diagnosis are separated from care planning and treatment, a significant proportion of services will be rendered through virtual channels.
Providers must ask themselves: How aggressively should we incorporate change? Should change just be additive? Or, does change allow for entirely new care models?
2. Innovators will complement – and, in some cases, supersede – traditional providers. We expect to see that partnerships between providers, payers, and employers will end up producing a wide spectrum of business models. We also expect a greater emphasis on serving consumers directly.
We’re already witnessing a proliferation of AI-based health applications. In fact, the latest version of the Apple Watch – to be released in late 2020 – includes applications for tracking heart rate, detecting irregular heartbeats, and capturing an electrocardiogram. The advancements over the next decade will be a parallel effort with two tracks. The first track is the continued design and development of AI-based platforms. The second track is about developing business models to deploy these platforms into the mainstream healthcare value chain to be adopted by all healthcare stakeholders. Consumers are already at the forefront of adopting wearable devices. However, translating these insights into appropriate responses will require clinical inputs and collaboration with providers. On the other side, innovators will need to collaborate with payers and employers to reimburse or finance these applications.
For innovators – especially if providers are slow to adopt – ask: What are our opportunities to establish AI-driven stand-alone service models that consumers can access?
The new Apple Watch includes applications for tracking heart rate, detecting irregular heartbeats, and capturing an electrocardiogram.
3. Life sciences and pharma will see significant improvement in the lifecycle of the research and development of drugs and therapeutics as AI accelerates clinical trials. Digital therapeutics will complement, if not replace, traditional medication therapies.
Pharmacy benefit managers have already incorporated digital therapeutics into their formulary for chronic conditions, such as diabetes and depression. Although it requires efforts upfront to develop medical policies and procedures for the review and authorization of such digital therapeutics, we’re already witnessing an uptick in adoption, with hundreds of thousands of patients leveraging digital therapeutics from AI-services providers such as Livongo, Omada, and SilverCloud.
For life sciences and pharma leaders, ask: Which digital therapeutics will truly drive value for patients? How do we prioritize? Because digital therapeutics – unlike traditional therapeutics – have a much shorter lifecycle for research and development, how and where should we prioritize the development of digital therapeutics?
4. For payers, AI will transform care delivery for members with chronic conditions and optimize network performance and clinical outcomes in a differentiated way.
New products and benefits will incentivize members and providers to adopt an AI-driven ecosystem (such as wearable devices) for monitoring and mitigating chronic health conditions and encouraging people to embrace healthier lifestyle choices. As AI improves diagnosis accuracy, it will reduce the overall risk of managing patients with chronic conditions. As a result, we envision a wide array of condition-specific subscription models. Alternative financing and funding mechanisms will emerge.
Regarding prior authorization, existing care guidelines will be supplemented by AI-driven, real-world evidence due to which manual review will be eliminated with minimal exception.
Regarding networks, what we consider provider networks will expand beyond clinicians, physicians, or typical ancillary-services providers (such as vision and durable medical equipment) to include AI-powered care models. AI-based service providers will be part of provider networks, warranting the need for new payment models and contracting requirements. Providers will be incentivized to refer patients to AI-based service providers.
Regarding risk management, new regulatory policies and risk management frameworks will mitigate liabilities tied to AI-driven decisions. This will enable differentiated underwriting and reinsurance approaches for payers with superior views of patient exacerbation risk.
Payers should ask the following questions: How do we want to shape the way these services are brought to the market? And how will they be incorporated into benefits? Can they provide new services directly?
5. Employers will see a wide array of options to contract with stand-alone service providers who offer AI-driven platforms and products to influence the quality of cost and care for chronic patients.
Regarding benefit redesign, the emerging AI-based service providers who partner with employers will mature. We will witness the widespread proliferation of these providers across the care continuum.
Regarding joint data ownership, employers will seek access to a wide range of member data gathered through wearable and monitoring devices to aid the mitigation of costs for chronic care management. In return, employees will receive incentives to adopt these wearable and monitoring devices and allow employers access to their personal health information.
Employers should ask the following questions: How do we incorporate these AI-driven platforms and products into our employee benefits structure? Which key platforms and products are most relevant for our employees? How do we source these?
AI must be viewed as a counterpart to existing resources.
Ideal Future Perceptions of AI
Given its potential, it’s inevitable AI will play a dominant role to help prevent acute events for patients with chronic conditions. However, given that the ability to harness AI’s potential and capture value is also so vast, that’s inevitable, too. It’s more about who will capture the most value out of this opportunity.
Transformation requires a concerted effort beyond data and technological capabilities. Change will involve a significant mental shift for both patients and providers to trust and integrate AI insights for early detection and diagnosis. AI must be viewed as a counterpart to existing resources. Above all, a holistic regulatory framework must be established to address privacy and security guidelines. AI transforming the art of prevention is no longer a matter of “if” but “when.”