As the largest provider of health plan services to the Medicare Advantage population, Humana helps millions of vulnerable individuals get access to healthcare. In recognition of the key role Social Determinants of Health (SDOH) play in successfully treating health conditions, Humana has launched the Bold Goal initiative. This population health strategy aims to improve the health of the people and communities we serve by making it easier for everyone to achieve their best health by addressing the root causes of health disparities.
As Humana’s Chief Executive Officer, Bruce Broussard, told Oliver Wyman last year, “Humana is investing heavily in advancing our clinical capabilities in five places we have the greatest influence – primary care, home health, pharmacy, behavioral health, and Social Determinants of Health – because these are our greatest opportunities to improve quality and health outcomes for individuals with chronic health conditions.”
Below, we offer an inside look regarding one of these five strategic pillars – Humana’s Social Determinants of Health initiative – in terms of where they are now, what brought them to this point, and what they envision happening next regarding their impact, scope, and sustainability as a thriving business model.
Q&A with Humana’s Andrew Renda
Parie: Your initiative to address Social Determinants of Health is called Humana's Bold Goal initiative. What is this goal about?
Andrew: Back in 2015, our CEO, Bruce Broussard, created a goal, which he intended to be inspirational, aspirational, and quantifiable. The goal was to improve the health of the communities we serve to make it easy for people to achieve their best health. The idea was to collaborate with local leaders, community-based organizations, providers, government agencies, and businesses to improve community health by 20 percent. The approach focused on addressing the root causes of poor clinical and social outcomes. We needed to identify the right metric to measure Health-Related Quality of Life - and also figure out how to achieve the 20 percent improvement.
One of our first exercises to do so was to evaluate some different Health-Related Quality of Life measures. We settled on the U.S. Centers for Disease Control and Prevention (CDC) Assessment, Healthy Days. Here, you measure how many mentally and physically unhealthy days people have over 30 days. We liked this because it was short, easy to administer, and was self-reporting by design. We also liked it because it gave equal weight to both physical health and mental health.
People answer a four-question survey about their health – questions that include “How many days in the last 30 have you been physically unhealthy?” And, “How many days in the last 30 have you been mentally unhealthy?” Then, you add how many unhealthy days you experienced in a month. This simple metric resonated with us, and with our members.
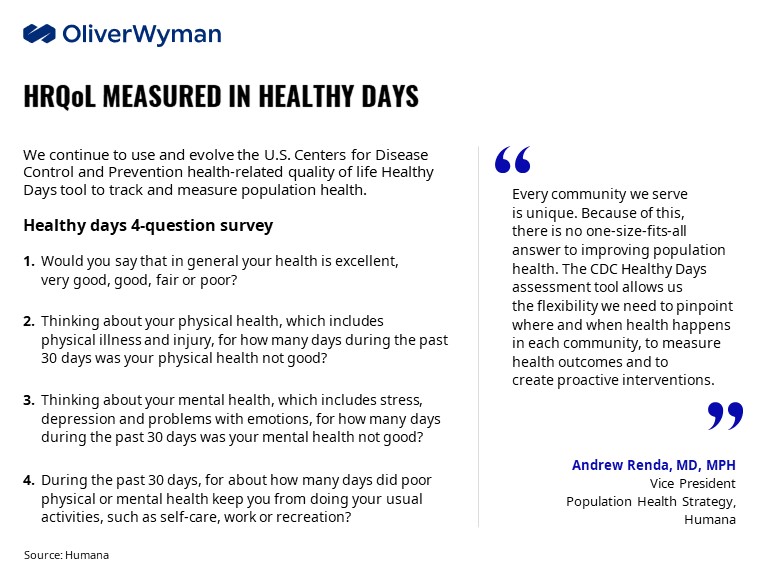
We wanted to go deeper and learn more about the impact of this questionnaire. When we went through some exercises in analytics, learnings, insights, and research partnerships, we found we first gravitated to chronic conditions. We were often saying things like, “Surely, somebody with complex diabetes or heart failure is going to have a lot of unhealthy days. That's certainly true.”
Then, in partnership with the Robert Wood Johnson Foundation, we began to understand the impact of Social Determinants of Health. Social determinants are conditions in the environments in which people are born, live, learn, work, play, worship, and age that affect a wide range of health, functioning, and quality-of-life outcomes and risks. Examples include social connection, food security, and financial stability. We found these determinants have an enormous impact on health status and quality of life.
According to our research with the Robert Wood Johnson Foundation, the number one health challenge seniors face is loneliness/inadequate social and emotional support. Number two was food insecurity. So, we started with those two and from there, developed analytics, intervention pipelines, and so forth. Now, we've gotten to the point where we're trying to scale work in those spaces, while also expanding out to other social determinants like transportation, housing, and financial security.
Parie: You mentioned Healthy Days' simplicity resonated with you. How have consumers and the broader market responded to Healthy Days?
Andrew: Consumers like Healthy Days, because it's easy to understand and it's personalized. It takes a complex thing like health or healthcare and boils it down to how health impacts an individual and their quality of life. For example, although a lot of seniors, in particular, may not understand hemoglobin A1C for diabetes control or the stages of Congestive Heart Failure, but they understand what a “healthy day” means to them. “You had 20 unhealthy days in a month. That means two out of three days for you are unhealthy, physically or mentally. So, let's work on that. Let's think about why you're feeling unhealthy and let's think about things we can work on together.” If you can say words like that, this represents an entry to a conversation. It's an entry to an engagement. It helps build trust. It says, “I care about you as a person. You're not just a condition.”
I think everybody wants to solve population health. But everyone defines population health differently. And, people have varying degrees of familiarity with Social Determinants of Health. So, we're helping define terms. And we’re helping with data architecture and infrastructure as well as the terminology around healthy days and social determinants.
Parie: I’m curious – what has Bold Goal’s impact been on the market so far?
Andrew: We have seen statistically significant improvement in Healthy Days trends, particularly in our Bold Goal communities, and also in our member’s overall health. But more broadly, we have advanced the idea that social determinants are really important to health and health outcomes.
Social Determinants of Health weren’t always considered something that should be part of our business strategy. The first time I presented to our management team on the topic of social determinants, I think some people in the room had never heard of the term. I think others had perhaps heard of the term but thought this kind of work was maybe something better suited for philanthropy groups, nonprofits, and the like.
But over the past four years or so, we've brought Social Determinants of Health into the fold as part of our clinical strategies and our business strategy. So that to me, is tremendous progress, because it’s a recognition that social determinants are so critical to health outcomes.
Did you know? Loneliness can be more dangerous for your health than obesity.
Parie: When you look to the future, what’s next in terms of your focuses?
Andrew: The next iteration for us is figuring out how to make this work sustainable and how to scale it both organically and through integration into our various business units. This will require more proof points - beginning with leading indicators - that show a return on health and a return on investment. This will then justify more innovation and bigger investments downstream.
For us, as a big healthcare company, we have multiple opportunities to integrate social needs into other aspects of our business. Because we are an insurance company, and we have insurance products for Medicare and Medicaid and so on, in some cases, we can incorporate social determinants into supplemental benefits. Examples of this are Value-Based Insurance Design (VBID) and Special Supplemental Benefits for the Chronically Ill (SSBCI). In other cases, we can work with physicians to incorporate social determinants into value-based care relationships.
Just before the pandemic took off, we launched a value-based payment innovation pilot centered around social determinants of health. The pilot has two goals: (1) determine whether incentivizing providers would lead to more screenings, documentation, and referrals to community resources, and (2) whether addressing SDOH actually improves patient outcomes, such as lower acute hospitalizations, reduced readmissions, lower ER utilization, greater healthy days, lower A1c, etc. Another way to scale this work is by treating social determinants as gaps in care within clinical scenarios.
At Humana, we have a comprehensive enterprise clinical operating model. We have telephonic nurses. We do in-home care. We do a lot of virtual care. Our objective now is to integrate social determinants, alongside clinical and quality gaps, into each of these clinical workstreams.
Parie: As you continue rolling out the Bold Goal initiatives, what lessons have you learned along the way?
Andrew: We’ve learned you can't design population health strategies from an ivory tower. You have to go “boots on the ground” to understand what's happening in communities. Data doesn't always tell the full story. You have to talk to people that live in those communities and have the experience. Community discovery and working with local stakeholders is critical to finding root causes as well as sourcing solutions.
I’ve also learned that to be taken seriously in the industry, we must treat social determinants with the same rigor that we've treated chronic conditions for years. And by that, I mean you've got to design studies around interventions. You've got to think about return on investment. You've got to think about leading indicators. You’ve got to test small and then have an innovation pipeline to be able to scale in different ways.
Parie: How has Humana's strategy evolved?
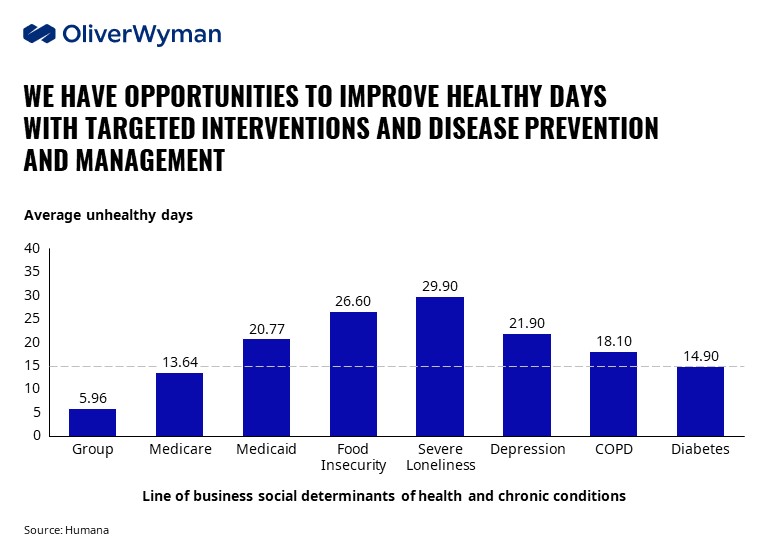
Andrew: The evolution of our strategy starts with this idea of a social determinant care continuum. One that includes prevention and risk assessment, clinical treatment, and social interventions. Then, in order to create a strategy and scalable model, we need to build upon the core. It’s kind of like the layers of an onion. You go one layer out from the initial strategy, and you have to think about creating infrastructure. And for us, that's largely data structure and about creating a data ecosystem for social determinants.
Regarding evidence-based scalable solutions – like pilots and interventions – it’s critical we have good study designs which include control groups and randomization. Then, we think about clinical integration and ways to scale.
That then gets us to the third layer out – a sustainable business model. Here, it's about understanding how you're accounting for costs versus the impact and the outcome. And, we need to identify the right sustainable model for social determinant operations – via supplemental benefits, value-based payment innovation, or something like creating a new social risk adjustment system.
So, that's how I think about it – going from this core care continuum of social needs, going out to building an infrastructure around it, testing and scaling solutions, and then thinking about how you make it sustainable from a business model perspective.
Did you know? Sixty-six percent of those experiencing food insecurity have to choose between food and medical care.
Parie: Are there particular pilots you’re trying out, given what you learned in the Bold Goal rollout?
Andrew: Yes. Over time, we’ve gravitated more towards addressing near-term health-related social needs like food insecurity and loneliness.
On that note, one partner we’ve done several pilots with is Papa – a company started in Florida. Their tag is “family on-demand”. They recruit college students to go into seniors’ homes – not for home health, but for companionship to help them address loneliness, social isolation, and things like that. It’s a simple solution, but it's so effective. We have seen statistically significant improvements in both Healthy Days and Loneliness scores.
During the pandemic, we had to pivot a little, because their whole model about going into seniors’ homes and having that face-to-face interaction made social distancing too challenging. So, we pivoted to some virtual visits. Then, we pivoted further with them to ask, “What if we could address two birds with one stone and have the Papa pals deliver groceries to food-insecure seniors?”
We’ve got to find the right solutions. We've got to figure out what has an impact. And then we've got to source capital and figure out how to get bigger and better and reach more people.
That’s our mission going forward: utilize the incredible power of sustainable teamwork.
Parie: Thank you, Andrew, for sharing your perspective and exploring how you’re working to transform healthcare. We look forward to seeing how the Bold Goal progresses over time and how your continued leadership efforts unfold.
.jpg)
.jpg)