We prepared our annual predictions before the recent partnership announcement from Amazon, Berkshire, and JPMorgan Chase. If anything, this news reinforces the long-term trends we’ve highlighted over the course of the year and suggests the transformations we envision might be coming faster than we thought! -- Terry Stone
2018 has arrived, and executives from healthcare companies both big and small hit the ground running. Just a few weeks after the New Year, our Oliver Wyman team was out in full force at the 36th annual J.P. Morgan Healthcare Conference (JPM) in San Francisco. Despite the soggy weather, optimism was in the air, with collaboration over cocktails, deals discussed over dinner, and coffee chats about what disruption for everything from new drugs to artificial intelligence might bring.
We also had the opportunity this past January to take part in the latest StartUp Health Festival – a groundbreaking event highlighting how true healthcare transformers are shaking up the industry.
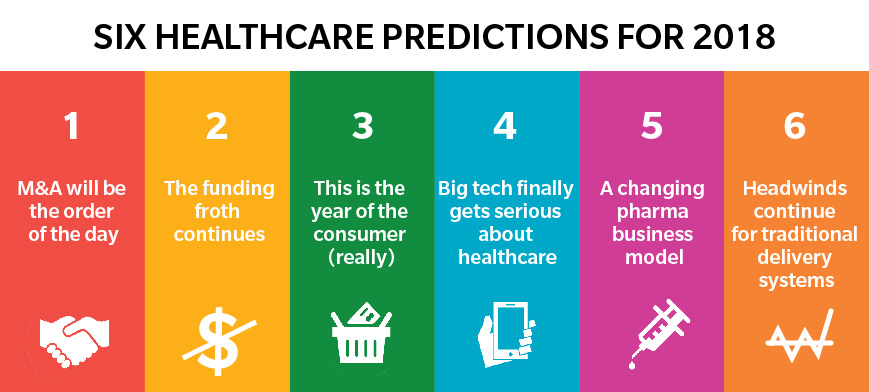
Here are our top six healthcare predictions for the year ahead, informed by our key takeaways from JPM and StartUp Health:
1. Mergers & Acquisitions Will Be the Order of the Day
There were many announcements late last year regarding some pretty major healthcare deals, including CVS-Aetna, Optum-DaVita, and Humana-Kindred. Although the industry has been talking about vertical integration and value chain convergence for some time, this talk is finally turning into action. As our own research shows, consumers take a holistic view of their healthcare experience – and the traditional structure of siloed insurance and care delivery simply does not meet their needs. With the more conventional horizontal combinations like Aetna-Humana and Anthem-Cigna failing to pass regulatory muster, payers are now on the hunt for consumer-centric diversification plays. Therefore, the coming together of care financing and care delivery will likely be just the ticket in 2018.
We are also likely to see more provider consolidation in 2018, with Catholic Health Initiatives (CHI)-Dignity and Advocate-Aurora having already announced combinations, and Providence and Ascension rumored to be in merger talks. As we see the value chain converging around payers, traditional delivery systems are betting that being bigger will help them hold their own against newly-integrated competitors. We will see whether or not that holds true, however. Assuming deals pass Federal Trade Commission (FTC) scrutiny (which is not a given), our experience shows that integration across markets and cultures will be a massive challenge. After all, 66-80 percent of merger & acquisition (M&A) deals fail to achieve their objectives.
All this activity is clearly underpinned by a favorable capital environment, with the recent corporate tax cut benefitting for-profit players, and companies newly able to repatriate oversees cash without a massive tax burden. This capital environment should benefit pharmaceutical companies in particular, and, despite lower deal volume in 2017, we expect 2018 will be an active year for drug company M&A.
2. But the Froth Will Continue
With plenty of capital available and more digital health startups popping up than ever before, there was tremendous buzz swirling at StartUp Health about funding rounds and which companies would be acquired next. But there were also more somber discussions about whether or not there is more funding available than there are good opportunities to invest – with the consensus being yes.
This phenomenon is partly because healthcare is hot – which is a good thing. When innovators and funders pay attention to an industry, disruption really starts to happen. According to Rock Health, 2017 was a record year for healthcare venture capital funding, with over $6 billion invested and the most deals over $100 million on record.
That being said, we kept hearing people talk at the Oliver Wyman Health Innovation Summit about Clayton Christensen’s “jobs-to-be-done” framework which, in brief, says consumers tend to make purchasing decisions not based on demographic factors like their age, race, or marital status, but because they need to solve a problem. Therefore, perhaps the biggest challenge disrupters will face this year is the management of too many point solutions. It will not be enough in 2018 to define your audience without defining the solution you offer for consumers. Healthcare leaders will therefore succeed when they can reach consumers already faced with far more apps, widgets, tools, and noise than they can handle.
Echoing GE Venture’s recent venture capital prediction that digital health has perhaps already reached its zenith, we agree digital health still struggles to gain traction. For instance, a study from IMS Institute for Healthcare Informatics reported only 36 out of over 165,000 digital health apps comprise nearly 50 percent of all downloads. This is not surprising, as healthcare is a massively complex and highly-regulated industry, offering a product most people only think of when they become sick, with incumbent players who have a lot to lose if the status quo changes. Innovators who do not understand the system and approach the market with technology-first solutions are destined to fail. Unfortunately, there are too many such innovators. In 2018, good money will continue to chase bad ideas, perpetuating the froth of 2017.
3. This is the Year of the Consumer (Really)
For many years, the industry has talked about consumerism largely in the context of apps, experience, and elective services. And these tactics, for sure, represent an important part of the “how” of consumerism. Now, the “why” of consumerism exists – the conditions under which those who receive healthcare act like true consumers, and shop on their own dime.
With average deductibles for 2018 individual policies pushing $4,000, and even those with employer-sponsored coverage being hit with family deductibles around $3,250, in 2018 consumers will mostly be spending their own money for healthcare. As a result, they will behave like they do when buying other goods – shopping for value and convenience, making tradeoffs about what is a need versus a want, and asking plenty of questions.
Those who have the most – and the most meaningful – touchpoints with consumers will be in a place to earn their trust (and their dollars!). With 83 percent of Americans living within 10 miles of a CVS store, 50 percent of households having an Amazon Prime membership, and Apple or Google being part of nearly everyone’s purchasing decisions, it is not a given that traditional healthcare providers will necessarily win in a consumer-driven world.
4. Big Tech Will Finally Get Serious about Healthcare
The threat of technology companies disrupting healthcare has long been a topic of industry discussion. Yet, to-date, it has largely been just talk, with a few failed experiments by big technology in personal health records and the like. But this is likely the year where big tech gets serious about healthcare.
For instance, take Google, where Ryan Olohan, Google Healthcare’s Managing Director, and Jim Lecinski, Google’s Vice President of US Sales and Services, shared some eye-opening statistics about Google’s role in health.
As we learned at StartUp Health, most Americans start by asking Google their health-related questions. And healthcare-related Google searches including the phrase “near me” are up 60x in the past five years. What does this kind of consumer behavior mean? It means healthcare companies may capitalize more on consumers’ online information – including their Google searches. As we learned at StartUp Health, those searches may not continue to rise at such a high rate for long, especially as Google gets better at tracking consumers’ locations and using this information to automatically suggest ways consumers can improve their health, in live time. Even though heightened transparency for consumers does not necessarily result in more informed consumers, the bottom line is companies like DeepMind, the artificial intelligence sector of Alphabet – a Google Parent company – will be looking more into how consumers can better understand who is accessing their healthcare records, and why.
Technology companies are now in the catbird’s seat when it comes to engaging consumers regarding their health, as Google, Apple, and Amazon all have dedicated healthcare teams (some more “secret” than others).
So why is 2018 the year for the big tech breakout in health? The convergence of retail, financing, and technology (such as CVS-Aetna and Amazon-Whole Foods) gives technology companies brand new consumer data and innovative touchpoints. Combine that with ready capital, plenty of digital health companies looking for an exit opportunity, and traditional players (particularly payers) in search of new types of partnerships, and it is clear we are approaching the inflection point.
5. The Pharmaceutical Business Model Will Start to Change
With drug prices reaching record highs, new lifelong treatments being developed every day, and a healthy innovation pipeline, drug costs were front-and-center at JPM. Yet the current pharmaceutical business model came into being in an era when drug costs and drug cost growth were sideshows instead of the main event for most payers and plan sponsors.
The old game of blockbuster profits for drug companies, competition for prescription volume among drugstores, and pharmacy benefit managers (PBMs) being a black box will start to fade in 2018. We will see drug companies continue to test the waters in value-based pricing, preparing for the day when they must move away from fee-for-service pricing (just as their medical counterparts are).
We will also see startups like Capsule (and potentially mega players like Amazon) redefine what it means to be a “neighborhood” pharmacy. And PBMs will be forced to prove their value and play a meaningful role in managing the total cost of care from the exam room to the mailbox – whether in a vertically-integrated way, like with CVS-Aetna, or in competition with startups like RxAdvance.
6. Traditional Delivery Systems will Continue to Face Economic Headwinds
2017 was a tough year for traditional healthcare delivery systems, with cost and reimbursement pressures increasing, and an uncertain legislative environment making long-term planning difficult. This was reflected in financial results across the country, so much so that Moody’s Investors Service downgraded the entire not-for-profit hospital sector. Over 70 health systems announced layoffs in 2017, and we should expect more in 2018.
This financial shakeout will separate the wheat from the chaff among provider systems. MACRA puts over $250 billion in Medicare reimbursement at risk, meaning only those systems truly proficient at value-based care will succeed. More broadly, the Medicare population is growing at several times the rate of the commercially-insured population, meaning that most systems can no longer afford to play the Robin Hood game, using commercial revenue to subsidize unprofitable Medicare patients. Combine that with entitlement reform (read: lower Medicare and Medicaid reimbursement) being at the top of the Congressional agenda for 2018, and it is likely going to be a tough year for US health systems.
So what to do? The systems that survive will slash cost across payer segments, and learn how to serve Medicare patients in a way that better meets their needs and permanently reduces total cost of care.
In summation, 2018 will an exciting year for healthcare. Of course, healthcare’s widespread instability means our predictions do not always come true (as proof, here is our assessment of last year’s predictions). But based on our recently acquired insights from JPM and StartUp Health, as well as other recent news this year regarding Aetna’s nearly 76 percent spike in quarterly profit, we think the industry is truly headed in the right direction for consumers, communities, and shareholders.