Editor's Note: The G20 in October held an event aimed at bridging “cooperation between public and private innovation players, startups and corporates on a global scale.” The G20 Innovation League brought together a variety of stakeholders, including venture capital funds, startups, industry experts and other decisionmakers. Oliver Wyman’s Akshay Agarwal was on a panel that homed in on five key areas where innovation can play a role in addressing major challenges across the globe, ranging from smart cities to clean technology. Here is a summary of his shared insights on innovations that will reshape healthcare in the coming years.
Healthcare worldwide is at an inflection point. Throughout the past two years, we saw new collaborations form between academia, industry, regulators, and providers. Barriers to adopting technology fell as clinicians and patients became more comfortable interacting on various platforms and regulators loosened the reigns on payments. But as the slide below indicates, we still face significant hurdles in the coming years.
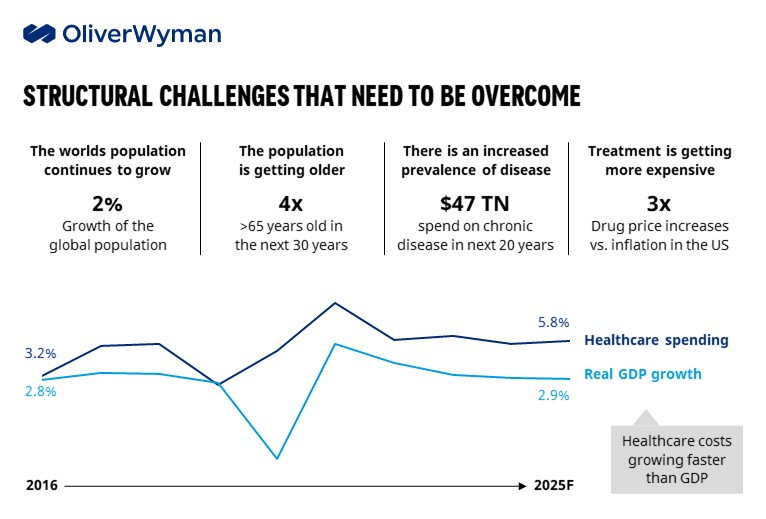
Creating a more sustainable healthcare system worldwide will require a fundamental shift in thinking and investment strategies. It will demand greater collaboration across all sectors and, critically, developing scalable solutions. Below are three areas that will shape the industry over the next five years:
Personalized care: There’s been a subtle, yet powerful, shift in healthcare over the past few years—referring to consumers rather than patients. It’s more than a change in vocabulary; it’s a different way of thinking about how care is organized and delivered. Healthcare has historically been a built around providers and physicians in a one-size-fits-all treatment and prevention model. Increasingly, consumers will be at the center of the equation and will demand more personalized approaches, and more convenience. Consider the impact of remote monitoring for patients with chronic conditions: Instead of traveling to and from a doctor’s office, they can upload vitals from their home and get tailored instructions in real-time from a multidisciplinary team.
Medications are moving in this direction, too. Personalized medicines accounted for 40% of molecular entities approved by the Food and Drug Administration in 2018, up from 5% in 2005.
Big data and analytics: Health systems have the capability to mine data in electronic health record systems to develop targeted solutions based on a growing set of clinical and demographic data, including how social determinants impact health outcomes.
The United Kingdom’s National Health Service, for instance, was able to identify and contact high-risk individuals within a few weeks of the COVID-19 outbreak. Similarly, in the United States, health systems were able to send mobile and pop-up vaccination events to high-risk communities.
Big data and advanced analytics are also being used to reinvent the way in which pharmaceutical companies discover new drugs, getting more potential candidates in the pipeline and lowering the failure rate of clinical trials.
Going digital: After a successful experiment, Ping An Insurance in China in 2019 expanded its network of one-minute clinic kiosks—small rooms where people can get a preliminary diagnosis and then be joined by a doctor on a video call, if necessary. The company put 1,000 units in place across eight provinces.
As clinicians and patients become more accustomed to these types of solutions, we’ll see technology used to augment the entire patient pathway, rather than having point solutions continue to drive a fragmented delivery system.
How might all of this come together in the coming years? Consider the following scenario:
A healthy 40-year-old tracks her health and activity on wearable devices and received targeted disease prevention advice. After feeling abdominal pains, she logs into a health app that asks a series of questions and advises her to keep monitoring her symptoms. If they go away in a couple of days, she’ll have avoided utilizing expensive resources. Her pain continues and she uses the app again, which now suggests she get some tests done. When the results come back, it reveals a gallstone and she’s referred to a doctor.
The physician uses robotic devices to perform a procedure. The patient returns home with a monitoring system that tracks her vital signs. Throughout the process, her data is uploaded into the EMR and the information is used to generate a prevention strategy to help ensure this doesn’t happen again.
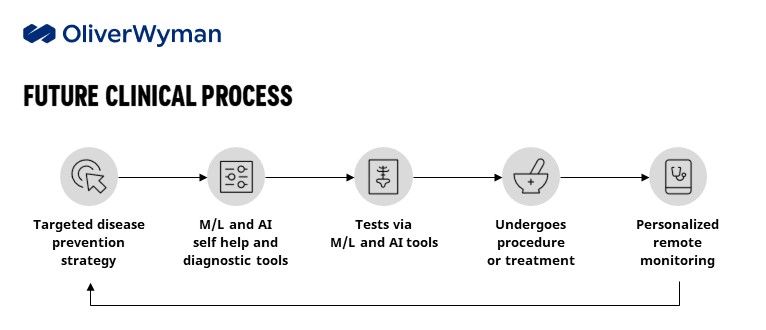
All these technologies exist today. Now it is matter of bringing them together for a more coherent, sustainable, and consumer-centric delivery system.