Editor's Note: This is Part 1 of a two-part series that was originally published on Medium. The topics below will be discussed in more detail by Oliver Wyman Partner, Dan Shellenbarger, in an upcoming conference hosted by Virta Health (September 29-October 1) called "Beyond Telemedicine."
COVID-19 has become a global nightmare, especially for people living with a chronic illness. The data paints a bleak and heartbreaking picture. According to the Centers for Disease Control and Prevention's (CDC) latest report on June 15th, hospitalizations are six times higher and deaths 12 times higher for COVID-19 patients with underlying conditions like type 2 diabetes.
The risk of COVID-19 infection, therefore, carries unbearable weight for the 50 percent of our population with a chronic illness, and is magnified for those seeking care in crowded clinics. Thankfully, federal and state governments have addressed this risk by relaxing telemedicine laws, eliminating the previously complex barriers to get licensed. People are now flocking to telemedicine to get care.
The power of virtual care for addressing chronic illnesses, however, was evident long-before COVID-19 began its assault on global health. Over the last four years at Virta, for example, we have seen our model of continuous remote care — near real-time access to dedicated physicians and health coaches — help thousands of patients transform their metabolic health, eliminate the need for medications, and reverse their condition, especially type 2 diabetes.
COVID-19 has accelerated the need for such models. Yet, unfortunately, most of the current discussion on the pandemic-induced move to virtual care obscures its true potential. If we are using telemedicine only to replicate our broken episodic, fee-for-service medical system, we are failing patients. This is the same system that has led to zero — yes, zero — improvements in population-level outcomes for people with diabetes (JAMA, 2019). The same system that creates a $400 billion diabetes cost burden for the US every year. The same system that causes over 200,000 deaths each year because of conditions related to type 2 diabetes.
So, even with the move to virtual care that we’ve seen thus far, we will still have 120 million people in the US living with pre-diabetes and type 2 diabetes in the wake of this pandemic. They will still face the same health risks before this whole thing started.
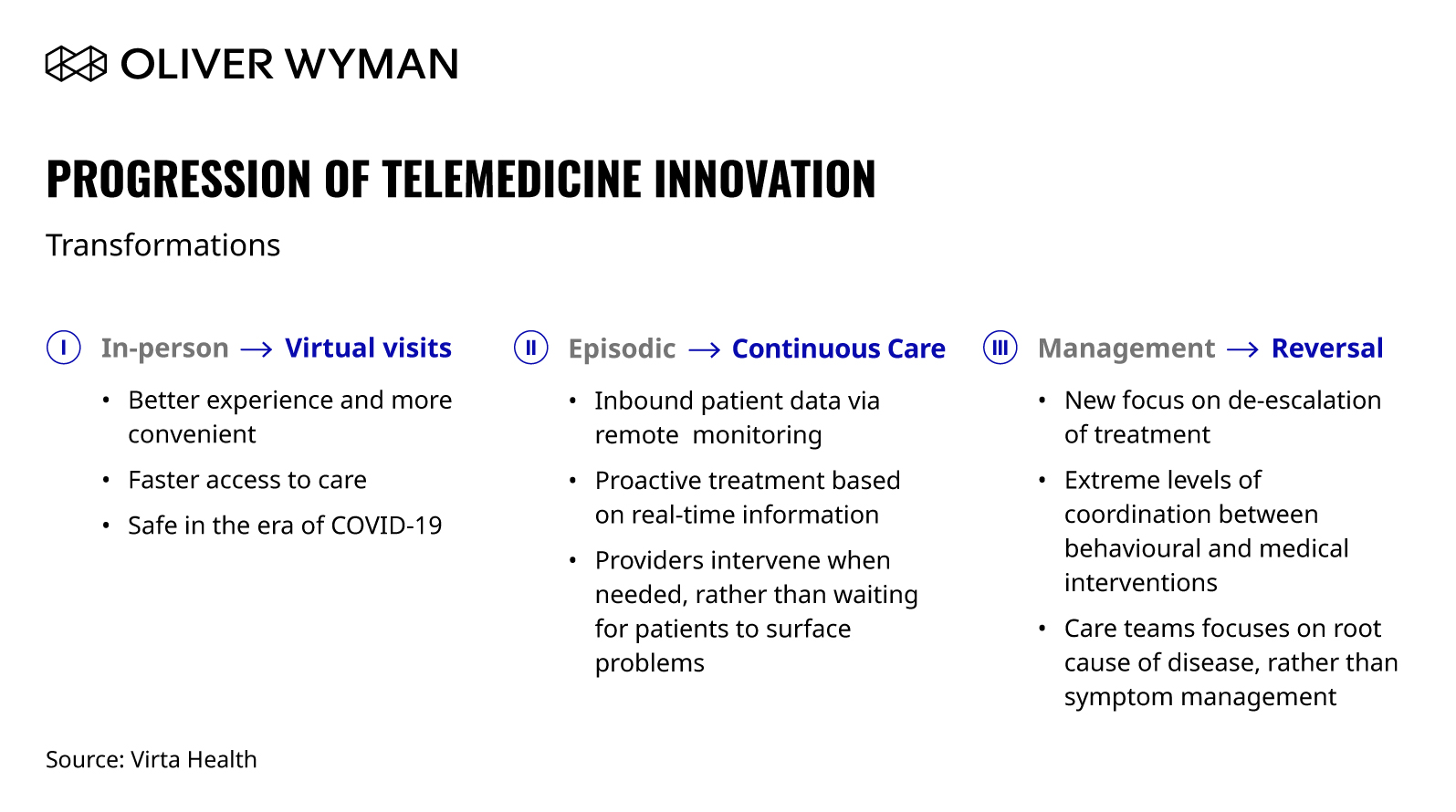
Unless, that is, we truly take advantage of this moment and seize the full opportunity that virtual care provides. Even with the drastically increased adoption and investment in the last few months, we are still early in telemedicine’s trajectory. I believe we are currently witnessing the acceleration of the first of three important transformations that, when fully realized, will reshape the healthcare industry for years to come.

 Share This
Graphic
Share This
Graphic
Progression of telemedicine innovation. Episodic virtual visits are just step one.
Transformation I: From In-Person to Virtual
This is where we are today for most of the “telemedicine” in the industry. Virtual-care delivery has been available for years, but with COVID-19, it has taken off in a way that won’t be unwound, and this is a good thing. Outside of being necessary for safety during this pandemic, it is much more convenient and provides a better patient experience. It opens the door to reach people in healthcare deserts, who are medically underserved.
But this is just scratching the surface. On its own, this episodic telehealth system won’t solve the growing chronic disease burden our nation faces, or radically improve health outcomes, or reduce our national healthcare bill. For that, the delivery itself needs to be changed.
Transformation II: From Episodic to Continuous Care
People with chronic illnesses live with their condition 24 hours a day, seven days a week. What to eat, what medicine to take, and how to manage symptoms are just a few of the minute-by-minute decisions that chronic disease patients make. Yet the prevailing healthcare model, mostly episodic, only lets them see a primary care provider for 15 minutes every three to six months.
A continuous model presents a radically new experience. Rich data coming from devices and manual input from patients gives licensed providers (if data is disconnected from care protocols and processes and those who need the data to make a clinical decision, it is more or less useless) orders of magnitude more information with which to make decisions. Symptom and medication management are turned into an ongoing collaboration and discussion that optimizes treatment for the patient. Ask any patient who has experienced this model, and you’ll hear how game-changing it is.
Meanwhile, it is well-known that lifestyle interventions can prevent and reverse disease. But, the misalignment of the care model to condition eliminates any hope of helping someone live disease-free. As a result, we write-off lifestyle interventions as “not sustainable.” Medical care and behavior change have thus been treated like two independent disciplines.
A continuous model of care changes this. Inbound data, analyzed by software, medical providers, and behavioral experts (health coaches), makes lifestyle interventions more sustainable and impactful than anyone ever imagined. For example, health plan leaders are often shocked when they learn that Virta retains nearly 9 out of 10 patients in its treatments after one year (contrast that to 40 to 60 percent medication adherence rates). This is only possible with a reinvented care paradigm.
This paradigm takes today’s healthcare system, which relies nearly exclusively on patients having to assess their own medical needs and schedule time with their provider, and flips it upside down. In this new, two-way, continuous, and data-rich environment, patients hear from their provider proactively. This dynamic cultivates the possibility of health outcomes that are inconceivable in our current system and leads to our third transformation.
Transformation III: From Managing Disease to Reversing It
The third transformation represents the true promise of virtual care: shifting away from disease management and toward prevention and reversal. At the heart of this transition is the de-escalation of treatment, where we focus on the root cause of disease, instead of the band-aid solution of symptom management, often with expensive drugs with many side-effects.
How is this possible? The technology advancements from the second transformation will make tight coordination between behavioral and medical practitioners commonplace, and drastically increase the frequency of interaction with patients. This collaboration opens the door for sustainable lifestyle interventions, which are nearly impossible with today’s, mostly episodic, practices.
These interventions are the antidote to the ongoing prescription of medications, which are no longer necessary with the right behavioral change. Importantly, this applies not only to type 2 diabetes reversal, but also other metabolic health conditions, such as high blood pressure, obesity, and dyslipidemia.
When this shift is fully realized, we’ll look back and wonder why we wasted so much time on managing symptoms, when we could have been reversing or preventing disease altogether. We hear this from frustrated patients all the time, who tell us they didn’t know a life without medications was possible until they found Virta.
In the near future, we hope everyone will know that reversing disease is an option, and one that is available now. COVID-19 has shown us how quickly we can advance and mobilize medical care when we have the will and need to do so.
There is no doubt we have the need, so it’s time for our industry to stop pretending that our current approach is going to fix the chronic disease epidemic. Change now isn’t just important, it’s a public health and economic imperative, and there’s no time to waste. A new healthcare system is right at our fingertips, one that provides better outcomes and is more just for everyone.


