Stars ratings often determine whether a Medicare Advantage plan is profitable, driving a bonus for top performers that accounts for tens or even hundreds of millions of dollars. At the best of times, Stars can perhaps be like a treadmill – payers may feel like they’re running faster only to have been standing still the entire time.
The COVID-19 outbreak is presenting even greater challenges for plans looking to close Stars gaps. The Centers for Medicare & Medicaid Services (CMS) is addressing this by changing the rules of the game for the 2021 Stars score (and possibly 2022, as well). In the meantime, unprecedented times are increasing amidst evolving uncertainty.
Despite Stars’ criticality to future success, many plans struggle to field strong programs that ensure consistently high scores. Designing and implementing a Stars strategy to drive score improvements is a dynamic process that requires constant attention from a team that has the focus and drive to adapt to rapidly evolving outcomes from the field. It’s not something you set and forget.
Stars Success Demands Stars Focus
Our experience continues to teach us that designing Stars strategies and programs turns out to be the easy part. Marshaling resources from across the organization to implement and continually drive the programs forward proves much more challenging.
If you’re not getting the results you’d like out of your Stars program, it may be due to the challenge of keeping everyone’s attention on something that isn’t the company’s main focus but is critical to the success of the business. Succeeding in Stars requires the close attention of departments and leaders from across the organization – including the Medicare business, provider relations, contracting, member engagement, information systems, technology, and beyond. But interweaving these kinds of different organizational sectors can prove challenging when each has competing priorities and directives.
Three Questions to Get a Sense of Your Future Stars Performance
1: Do you have 100 percent dedicated Stars leadership reporting to either the Medicare leader or the company’s executive team?
Often, the head of the Stars program, particularly in smaller plans, is the same person who oversees the Healthcare Effectiveness Data and Information Set (HEDIS) and/or quality programs across all lines of business. While HEDIS is a necessary component of Stars, it’s only one part of the picture. And, given CMS’ latest announcements, it will likely decrease in importance over time as the focus shifts toward member experience outcomes.
Also, Stars is very different from a commercial quality program, with a distinct population, unique measures tailored to a senior population, and constraints from CMS that require different approaches than a commercial program typically implements. Also, small population sizes tend to make it difficult to get providers to focus on the gap closure activities and even the incentives offered to drive performance.
Given the year-round, intense activity required to drive Stars score gains, this program requires a dedicated leader whose sole focus is designing and implementing a Stars strategy rooted in deep analytics. And, someone who leverages all resources at their command – whether from within the organization, from vendors, or from the provider network – to close gaps and improve measures.
This leader should be accountable to the head of the Medicare Advantage business or even the executive team. This way, their time and energy aren’t diverted away to support non-Stars activities.
Regarding one example of innovation, one of our large regional clients brought in an experienced Stars leader from outside the organization. This person’s ability to institute a strong process and accountability structure drove significant improvements in their measure outcomes, getting the plan back over the four-Star threshold they had lost just the year prior.
Conversely, another client that implemented a comprehensive new Stars improvement strategy but was unable to make the kinds of organizational and governance changes required to effectively oversee the strategy is still trying to get back over the four-Star threshold.
2. Does your Stars leader have real authority over matrix functions?
Unlike many other programs within a health insurance company, Stars requires active and energetic collaboration across multiple departments to be successful, without the benefit of having those departments accountable to Stars leadership.
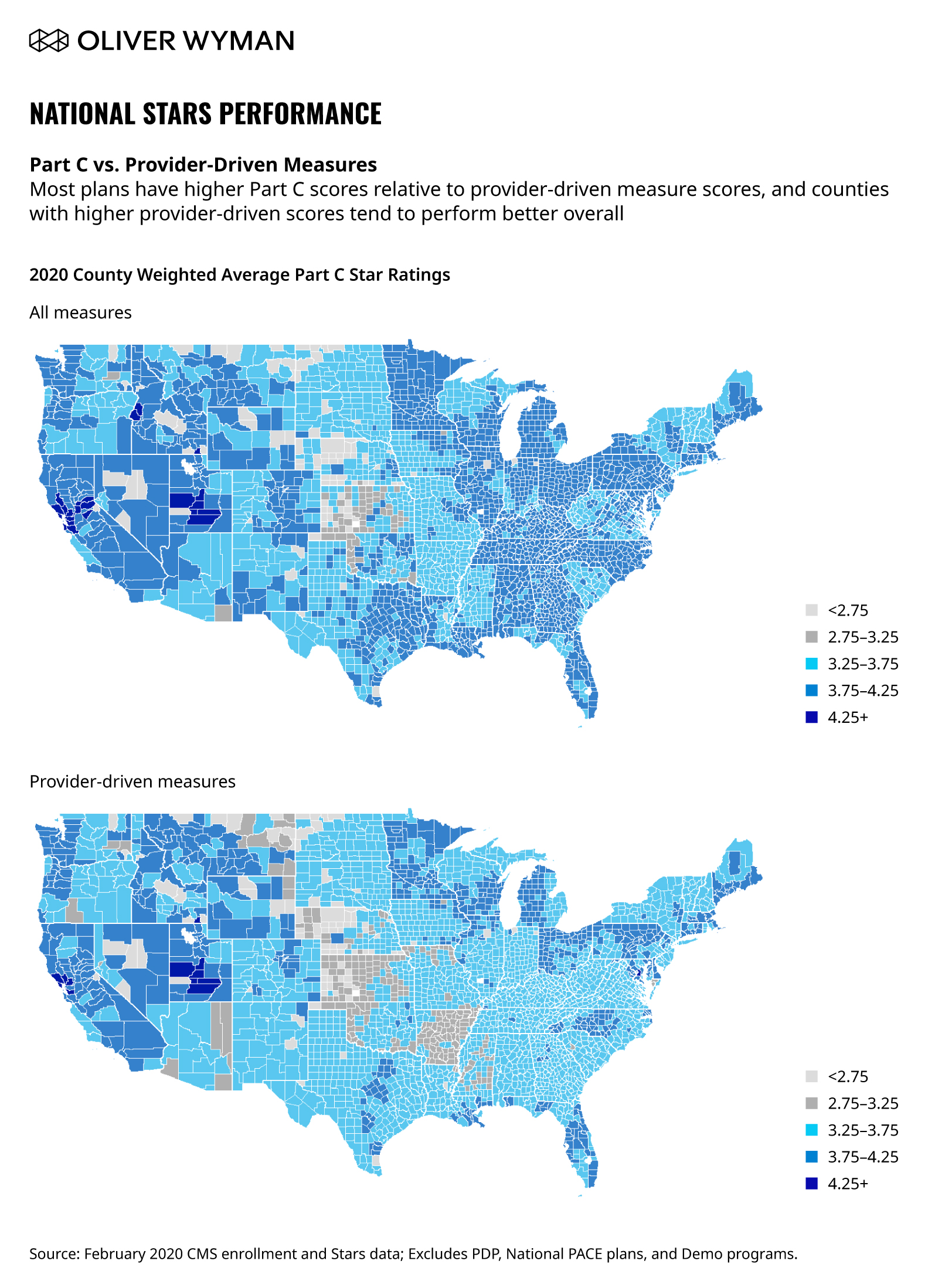
Provider relations in particular are critical to a Stars program’s success; as go the provider-driven measures, so goes a plan’s overall Stars score. Driving these measures requires close collaboration and cooperation from the provider network.
Provider-driven measures are a very strong predictor of overall Stars performance. Given the relatively small size of the Medicare Advantage book in most multi-line insurers, the functional teams – and the provider team, in particular – tend to focus on programs for the commercial population. This makes it difficult for the Stars team to get the attention they need to improve performance. The small numbers of Medicare Advantage members in a provider’s panel often makes the incentives too small for a provider to focus on, and plans will often require new processes or tools from the provider that are not worth their effort, thereby requiring a more nuanced approach provider engagement.
Designing a matrixed structure – and making sure the matrix functions appropriately – to provide Stars leadership with the appropriate points of accountability in each of these functional areas is key to effectively implementing a winning Stars strategy.
3. Do you have corporate-level Stars incentive structures in place?
Too often, Stars leadership is incentivized based on partial program performance. For example, incentivizing according to how many measures showed improvement versus the previous year or according to the success rates of specific gap closure programs. In contrast, the metric that matters most is the overall Stars score.
Even more importantly, the incentives are rarely applied across the organization. Instead, they are concentrated just within the Stars function – or at most, across the Medicare Advantage leadership team. Rather than taking on this kind of limited approach, the entire organization needs to be incented on Stars performance. This is because your Stars performance is not going to change unless you have corporate-level incentives that apply across all departments and that have an influence over the Stars score. If leadership is appropriately incented based on the overall Stars score, the programs required take on the importance and get the attention needed to attain that four- or five-Star target.
Don’t let your great Stars strategy and investments go to waste. Get the right people and the right structure in place to get the results your program was designed to drive.