Editor’s Note: This article is part of Oliver Wyman's ongoing series about the evolving novel coronavirus (COVID-19) pandemic.
It was perhaps much easier shutting down the world this year in the face of coronavirus than it is to re-open the world. We’ve learned that although social distancing works – and works well – to flatten the curve, it can also be economically catastrophic.
COVID-19 is far from over. When you look at the nationwide numbers, there’s very little difference between the end of March and the end of May. Some states still haven’t hit their first peak yet, let alone a second peak, either because they re-opened when their case counts were still rising, or because they mistook where they were on the slope of the curve, and cases in fact plateaued before continuing to rise higher as states re-opened. According to Oliver Wyman analysis, as of June 18, 40 percent of US states had week over week growth in new daily cases, particularly in the South and the West. California, for example, has seen a relatively steady rise in active cases throughout the pandemic, while states like Texas or Arizona appeared to be at a plateau, but have seen rapid recent growth. In other cases, particularly rural states like Alaska, Idaho, or Montana, confirmed state-wide cases fell before rising higher towards what may eventually become a second peak.
Can we find a way to balance interacting with one another – at least economically – with the right public health measures to keep the virus from spreading too rapidly and overwhelming local hospital systems?
To help make sense of this question, Helen Leis, Partner in Oliver Wyman’s Health & Life Sciences practice, who has worked with the Centers for Disease Control and Prevention (CDC) to develop their pandemic preparedness and response protocols, shares her views on smart containment below in a Q&A with our editors.
Oliver Wyman Health: What are we learning regarding all the COVID-19 testing that’s being done?
Helen: Testing and contact tracing are components of a smart containment program. Testing tells you how prevalent COVID-19 is in a population and how fast it's spreading; contact tracing allows you to rein in a cluster of cases before they become a full-scale outbreak.
Some testing guidelines have been put in place to help better determine how hard the virus has hit specific regions. The World Health Organization (WHO) and others, for instance, established certain required benchmarks saying that less than 10 percent of tests across a region should come back COVID-19 positive. So, if you’re getting twenty or thirty percent of tests coming back positive – like we saw in New York about a month ago – that’s too high and means you’re largely just testing people who are experiencing symptoms.
Massive testing at scale helps contextualize the disease’s severity. For example, countries like Germany and South Korea have performed widespread testing; when calculating their case fatality rates (number of deaths from COVID/number infected with COVID), the denominator is larger than for other countries who aren’t testing as much, resulting in a lower-case fatality rate. But testing also reduces economic pressure. Testing provides people – like consumers and employees – comfort and confidence through transparency.
This is critical. According to Oliver Wyman analysis, for example, consumers were hesitant as of late April to re-enter public life, with 72 percent of US respondents saying they’re not yet comfortable going to a place with crowds, like a subway, theatre, stadium, or restaurant.
Oliver Wyman Health: Consumer hesitation and all that comes with that is still prominent. How much has changed since COVID-19 first hit the US? Just like it was a few months back, there’s still no herd immunity, no vaccine, and limited treatment options.
Helen: Despite the fact that it feels like March the 107th, we’re still living in the early stages of this pandemic. We’ve witnessed states re-opening across the country for nearly two months, and we can now turn our attention to figuring out how we can go about our daily social, economic, and public lives and how smart containment can limit future case growth while minimizing economic damage.
We’ll need something more surgical than the one-size-fits-all blunt lockdown approaches we used in the spring. Instead, we’ll want to adopt a more segmented approach to shield the most vulnerable – the elderly and those with compromised immune systems – and allow those who are less likely to suffer serious illness to circulate in society with some safeguards in place.
Oliver Wyman Health: Since so many people are spreading the virus and don’t know they’re doing so, what kind of testing approach is necessary to protect more people?
Helen: Multiple studies point to the asymptomatic transmission of the disease – in some studies as much as 40 percent of cases. Therefore, testing can help us achieve two objectives.
The first objective is more directly oriented to public health. If a proportion of confirmed cases is asymptomatic (and perhaps even a larger proportion still of the “undetected” cases), then testing is important to identify those folks and ask them to take precautionary measures to protect the people around them (such as isolating for a period of time), and allows those who have not tested positive to continue to go about their business (also while taking precautions like wearing masks in public). A robust testing strategy goes hand in hand with contact tracing of course, which we’ll talk about more.
The second objective of running extensive testing is a bit more psychological. By testing widely, you can give people – consumers and employees – a sense of comfort, that we know how pervasive – or not – the virus is in a particular geography or even physical location (like a distribution center or a plant), and to what extent it’s safe to go about your “normal” routines in public. If, say, between two and five percent of COVID-19 tests in the geography are coming back positive, people can feel comfortable that the virus is less prevalent and the local authorities have it “under control.” If it’s more like 40 percent of tests are running positive, then we know that the virus is more pervasive and we need to take greater precautions.
Oliver Wyman Health: Let’s go back to contact tracing – why is it valuable?
Helen: Contact tracing is simply identifying individuals who have come in contact with an infected individual up to two days before the onset of his or her symptoms. The contact tracing is important because it allows you to pounce on an outbreak as you see it emerge, rather than watching the percentage of positive test statistics rise and then realizing too late that you may have a wildfire on your hands.
Contact tracing lets you know more about how many others may also have been infected by one person’s positive test. And we’re learning more every day about how heterogeneous the transmission of the virus is – one person may infect many, while another could infect very few.
Let’s say three sisters all test positive for COVID-19. What did their lifestyles look like right beforehand? Maybe the first sister was social distancing, hunkered down at home save for staying within the confines of a large backyard, therefore not coming in contact with anyone else. Maybe the second sister went for a daily run (where she was careful to maintain social distance), but sometimes was joined by a running partner, who now needs to get tested, too. But the third sister went to a birthday party with 30 people, so now all 30 people need to get tested and their contacts traced.
"Despite the fact that it feels like March 107th, we’re still living in the early stages of this pandemic."
Oliver Wyman Health: Why does contact tracing seem so much more difficult and labor-intensive with COVID-19 than it is with other diseases? When it comes to a standard sexually transmitted infection or something like Legionnaire’s, the difficulty of contact tracing for COVID-19 is drastically different, in comparison. Why?
Helen: There are a few reasons. When it comes to contact tracing for a sexually transmitted disease (STD), or something like Legionnaire’s, those investigations too can be difficult, either because you are having to ask patients sensitive questions about the kinds of activities they may have engaged in, and they may be less forthcoming, or because you are having to go back 14 days and investigate their activities and exposures to determine the source of Legionnaire’s – typically a water source contaminated with Legionella bacteria. So you’re tracking symptoms of cases, against activities of cases. COVID is tricky to trace for a number of reasons: the virus preys on crowds in close proximity in enclosed spaces. When you have a person who tests positive for COVID-19, the CDC’s guidance is to contact tracing any person who was within six feet of the individual for more than 15 minutes in the two days before symptom onset. So if you took a subway, or bus, or went to a play, you probably had a lot of people within 6 feet of you, and you likely knew none of their names (ok, maybe one or two). So the tracer has to figure out who else was in your vicinity – a daunting task.
Some countries like South Korea and Singapore have tackled that by leveraging a number of technologies and databases – credit card data, mobile phone data, GPS tracking technology – to pinpoint the strangers who sat in front of you at the play. But those technologies come at the expense of privacy and some individual liberties. The other aspect of COVID-19 that makes tracing more challenging is the fact that we’re seeing asymptomatic transmission. Let’s talk through another example … Perhaps you are showing symptoms, and you test positive for COVID-19. The tracer asks where you’ve spent the 48 hours before your symptoms began. You attended a friend’s birthday party the night before at a restaurant. You knew some of the guests, but not all. You don’t recall anyone showing symptoms. So now the tracer has to get the guestlist for the party, confirm which restaurant staff were working that night, and ask them all to be tested to determine who transmitted the virus to you. That may take a few days, and in the meantime, those folks may be continuing to circulate in society and potentially spread the virus to others – this is why we saw it spread like wildfire in the early days.
Now that we are seeing more geographies implement measures like requiring masks in public, keeping social distancing in public places, and the like, we have some additional ways to pump the brakes on transmission.
Oliver Wyman Health: How do you envision digital tracing as you described in South Korea working across Western countries?
Helen: In Western countries, and particularly in the US, we walk a fine line when it comes to data privacy and individual liberties. There will perhaps be a hybrid one day of how apps ultimately trace people.
There's now proximity tracing that uses Bluetooth and specialized apps to identify individuals who were nearby for a prolonged period with an individual who later tests positive. Singapore has it. Europe and the US are planning to do it through a jointly developed Apple-Google tool. It could certainly help us – it allows us to trace faster than the “shoe leather” detective method, and still protects individuals’ privacy. The theory is it can maintain a high degree of privacy if it uses the DP3T protocol – which is what Apple and Google are planning – but it takes a lot of uptake. At least 60 percent of people need to opt into it for it to be effective.
Where Western countries perhaps get the most nervous is regarding surveillance infrastructure integration where you're harvesting data from closed-circuit television (CCTV), cell phone data, badge swipes, payments, and the like. This is what South Korea has largely done, combining lots of different data sources to trace cases and figure out where you were.
Oliver Wyman Health: I see. Beyond South Korea, what other countries have done an exceptional job, in your eyes, of testing and contact tracing?
Helen: Taiwan, Germany, Norway, and New Zealand. Interestingly, they each applied slightly different strategies. I can’t help but notice they’re all run by women. We saw in our diversity research 18 months ago that diversity drives more careful information processing – something I suspect is particularly valuable in times of crisis like this.
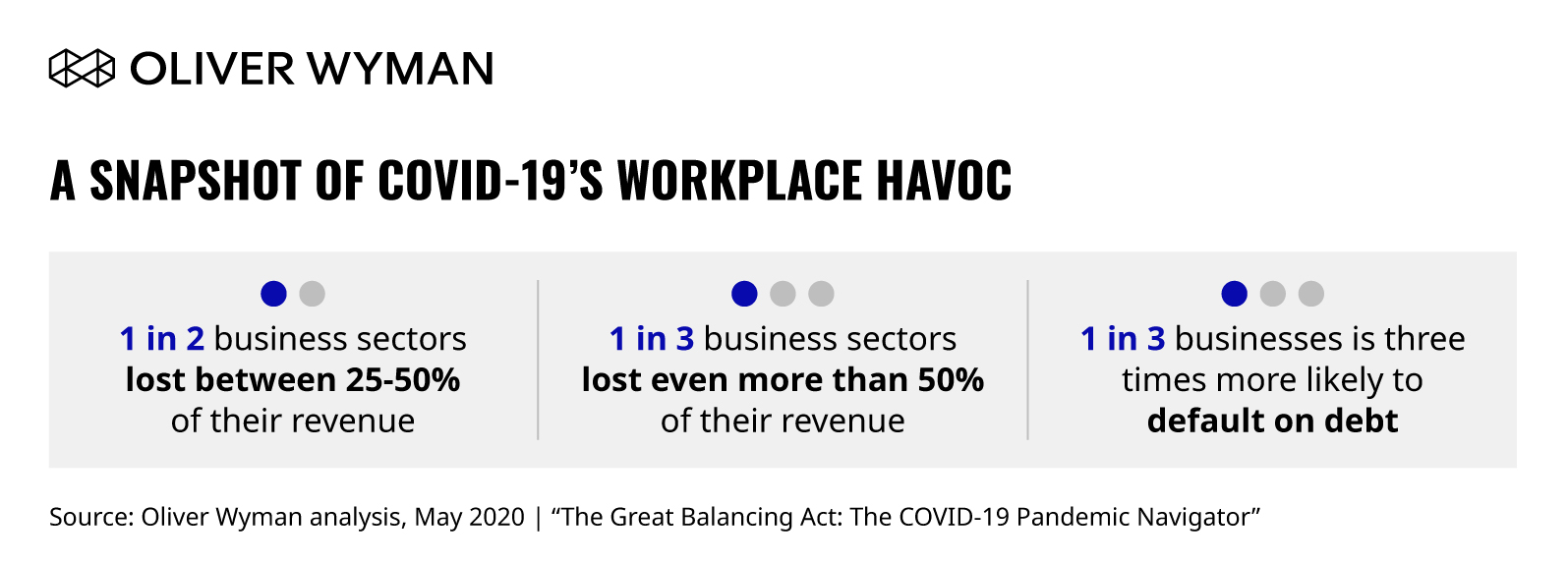
Oliver Wyman Health: Let’s switch to another topic about the public perception of COVID-19. According to Oliver Wyman's research from May, for example, more than one in two American consumers is not comfortable staying in a hotel (52 percent) and not comfortable dining in a restaurant (54 percent). What role do smart containment efforts, like in the charts below, play in strengthening the economy?
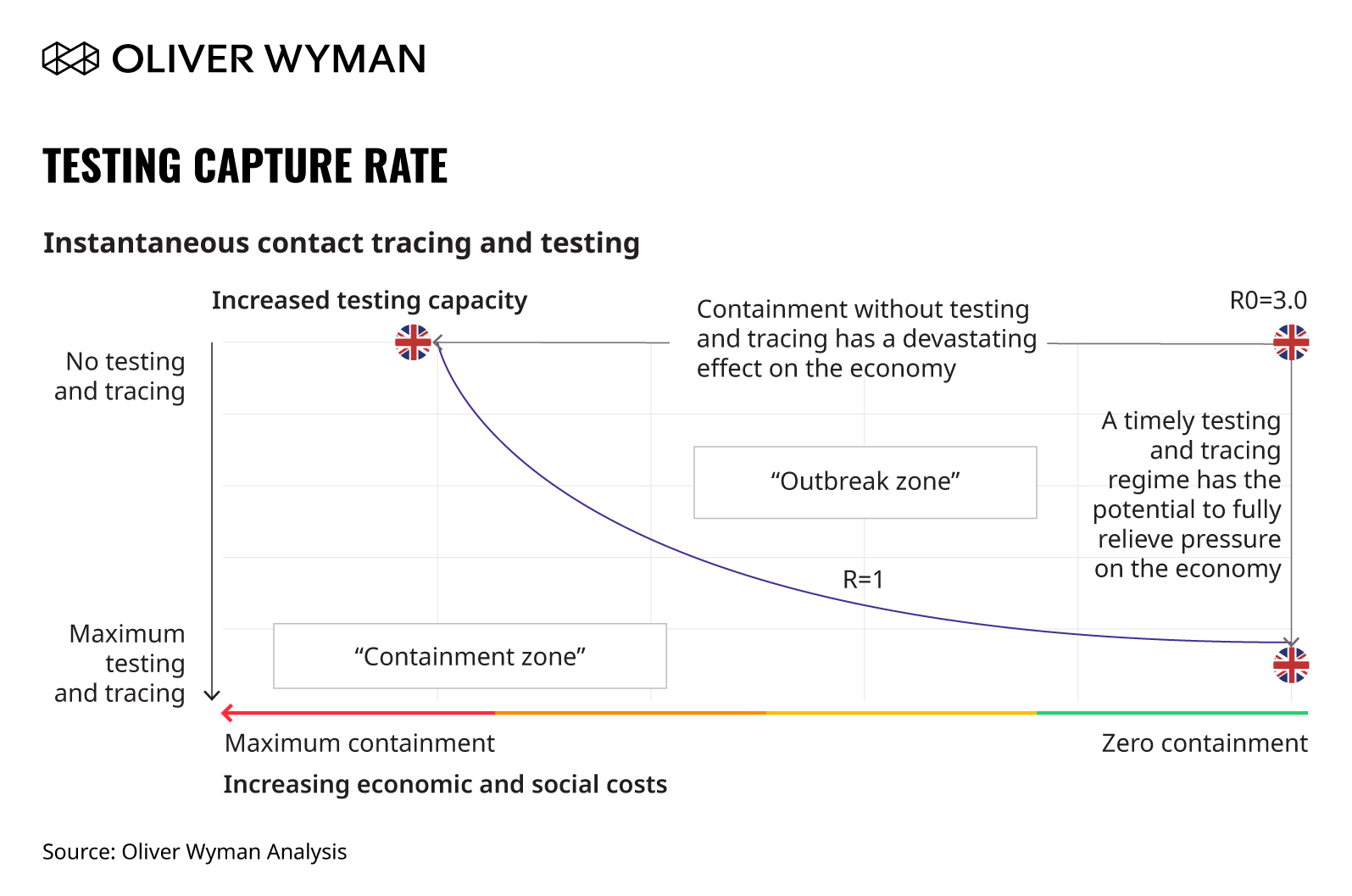
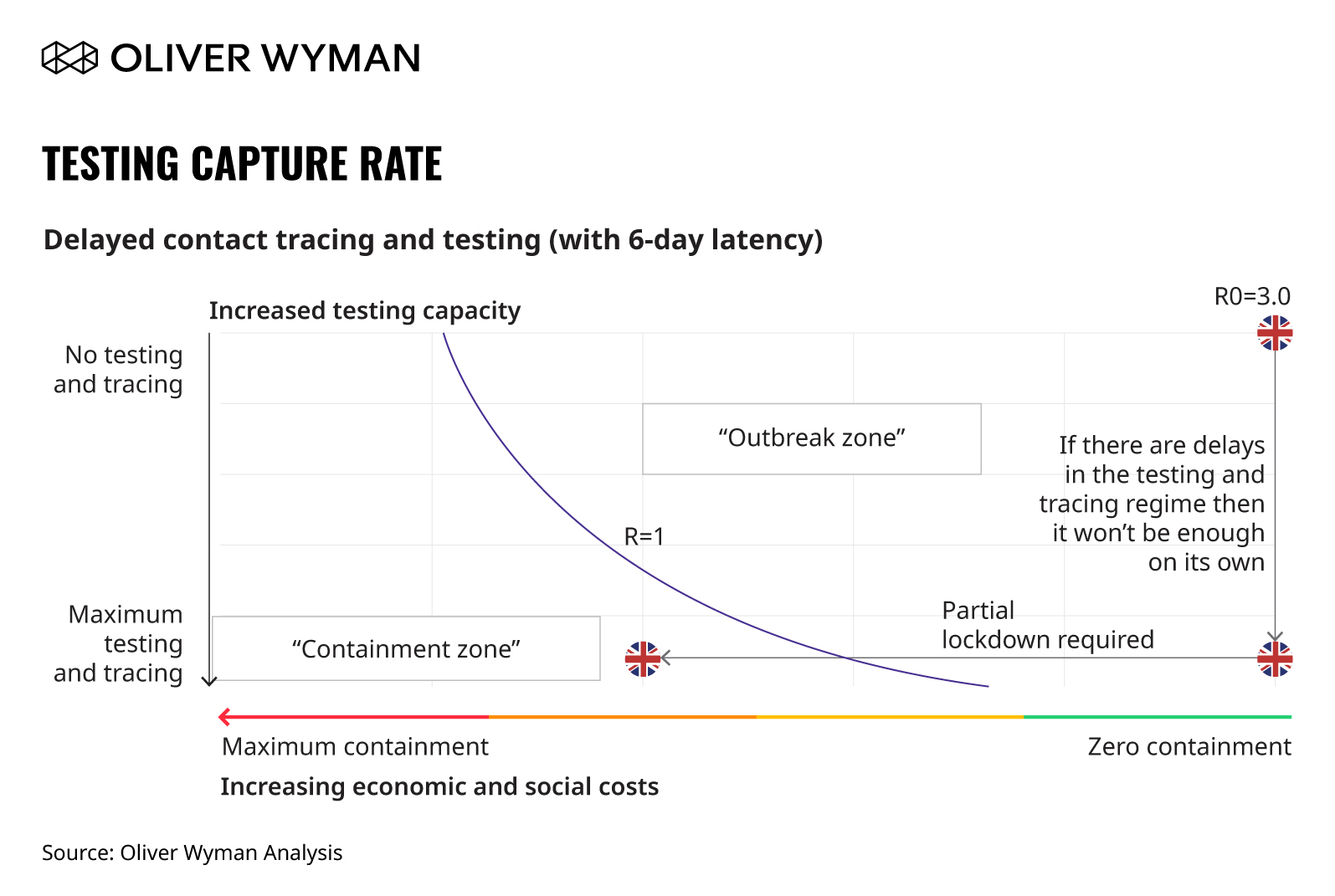
Helen: Some of it goes back to what I mentioned before about testing having a psychological benefit as well. If you are deciding to travel somewhere, and you see the positive test rates are low, and confirmed case counts are declining, and the local authorities have implemented a number of measures to protect people (I’m just going to keep beating that “masks in public” drum), then you may feel more comfortable checking into a hotel there. As we move into the next phase of containment, we must also look to differentiate our approaches by sub-region and by age groups in the population.
This is a big shift from where we are now, and from where we were in the very recent past. Not long ago, in March, for example, we didn’t have sufficient COVID-19 testing and tracing in place yet in many geographies, and instead, we had to look to heavy restrictions for entire populations. In many places, we didn’t have enough tests, so only those symptomatic patients in hospitals, where we needed the diagnosis to confirm which treatment to pursue, were tested. For people to begin safely circulating again, we needed to scale sufficiently to ascertain how pervasive the virus was, and ask those who were infected – even mildly symptomatic or asymptomatic - to take steps to slow the spread of the virus.
Testing and contact tracing, when paired with targeted quarantine for those who are contagious, is the frontier along which you can “play” with containment and relieve the economic burden posed by blunt force lockdowns.
Smart containment allows public health and economic health to be more in balance. I believe some folks have painted a false choice between economic health and public health. We’ve seen many sectors shift increasingly to a digital economy but much still depends on proximity to a customer (or a factory) to deliver. I’d argue that if consumers and employees don't feel confident enough in public health to go out, then it will be difficult to drive economic health.