The sudden and meteoric rise in use of new weight-loss drugs put a spotlight on obesity prevention. But decades before Wegovy and Ozempic took the market by storm, public health agencies ranging from the US Centers for Disease Control and Prevention to the World Health Organization had deemed obesity an epidemic. The crisis shows no sign of abating — the World Obesity Federation reported that more than half of the world’s population will be obese by 2035.
A set of interconnected challenges face patient segments, including lack of awareness around health risks, pervasive stigma, inadequate treatment coverage, and limited long-term monitoring options. Recognizing the urgent need for action, key stakeholders — patients, healthcare professionals, payers, and drug manufacturers — need to re-evaluate their roles for treating the disease and find new ways to collaborate to alleviate the burden of obesity on individuals and society.
Global obesity epidemic will surge by 2030
The WHO describes overweight and obesity as an abnormal or excessive accumulation of fat. A body mass index over 25 presents a risk to health.
Globally, the number of obese people ages five and older is forecast to reach 1.5 billion by 2030, with over two billion overweight people in the same period. The prevalence of obesity is expected to continue growing, more than doubling over the next few decades. North America accounts for the biggest proportion of obese patients, with roughly 41% of adults falling into that category. Countries across Africa and Asia are also seeing obesity levels rising fast.
Exhibit 1: Estimated prevalence and number of cases of obesity in adults (BMI ≥ 30 kg/m2) by 2030
Source: Oliver Wyman analysis
The rise in obesity rates has been linked modern lifestyles with issues ranging from poor nutrition, reduced physical activity and exercise, and poor sleep patterns being front and center. However, this narrow perspective on what contributes to obesity can lead to stigma and limit open dialogue around the health risks associated with obesity as well the need for medical intervention.
Obesity is a systemic issue and creates risk factors for a host of other conditions. It is associated with high morbidity and mortality risk and puts people at elevated risk from other health conditions ranging from skin disorders, heart failure, several types of cancers, and behavioral health concerns. In addition, at least 2.8 million adults die each year globally because of being overweight or obese. Studies suggest obesity could overtake tobacco smoking as the biggest cause of preventable cancer in the future.
Exhibit 2: Comorbidities associated with obesity
Source: Oliver Wyman analysis
Despite these risks, many people lack awareness about the complications associated with obesity. A recent study of overweight and obesity patients, nurses, primary care physicians, and public health experts found that most participants were unable to visually determine at-risk patients. In addition, most of the patients surveyed had limited awareness of health risks associated with obesity except major cardiovascular risks.
The growing nature of the problem, severity of the condition, and limited understanding about associated health risks highlight the need to assess the problem of obesity more holistically – from prevention to treatment. It is also important to consider overweight patients since they are at the highest risk of developing obesity in the future if not carefully managed.
Obesity patient populations face different sets of challenges
The hurdles faced by people with obesity or at-risk of obesity are distinct and a deeper assessment can help develop strategies to address them.
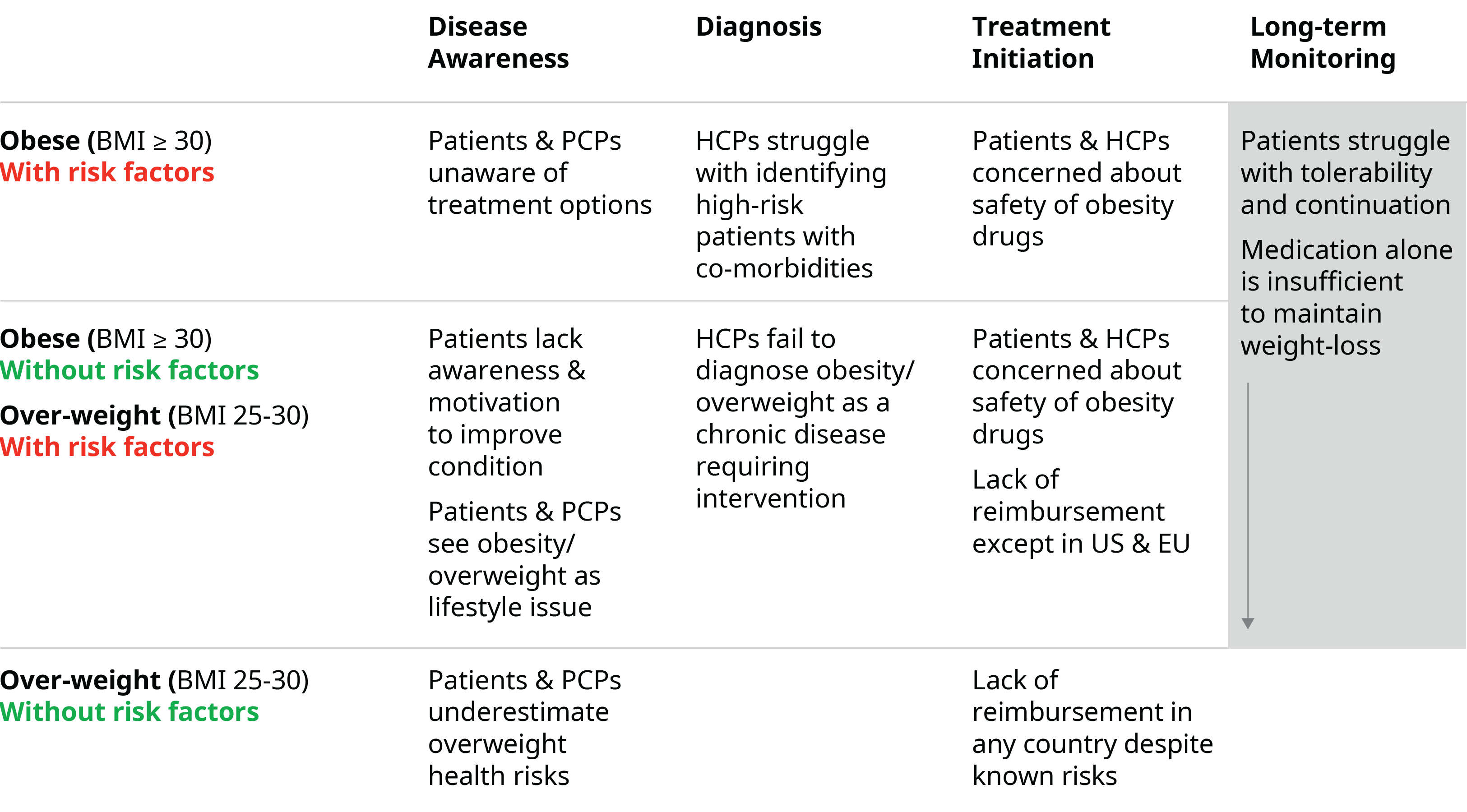
Exhibit 3: Obesity treatment challenges by patient segment
Source: Oliver Wyman analysis
Disease awareness: Obesity is often considered a lifestyle issue, leading to an underestimation of associated health risks, including in overweight patients. In addition, patients and healthcare professionals, especially primary care physicians, lack awareness about obesity and associated health risks. Patients can also struggle to make behavioral and lifestyle changes to improve their condition without guidance and motivation.
Diagnosis: Obesity remains severely underdiagnosed due to stigmas associated with the disease. Disease diagnosis is based on an imperfect body mass index measurement, which means patients with BMI<30 but with associated risk factors are not likely to benefit from obesity management and treatments.
Treatment initiation: Treatment decisions should be based on such agreed treatment goals as weight reduction or improved BMI and should consider behavioral and mental support along with any pharmacological interventions. Obesity medicines have historically had safety concerns that impact perceptions of using medicines, even in patients who are at an elevated risk for being obese or overweight. Inadequate coverage for obesity and overweight patients also poses a challenge. For instance, reimbursement of anti-obesity medicines by public health or insurance in Europe is very low — about 1% —with no or partial coverage in many countries. Private payers in the US use various mechanisms such as prior authorization or non-preferential formulary placements to restrict access. And the nation’s largest payer, Medicare, currently prohibits coverage of anti-obesity drugs for seniors.
Long-term monitoring: Obesity is a chronic condition and tolerability to long-term treatment can be difficult. There is growing consensus among experts that medication alone is sufficient to achieve and maintain obesity treatment goals – behavioral support, diet guidance, positive reinforcement, and regular monitoring and follow-ups are crucial to achieving treatment goals and long-term benefits.
Health system stakeholder roles need to change
Industry stakeholders must reconsider their role to support a holistic solution-oriented approach. Below we examine how various segments can reorient around a more comprehensive strategy.
Patients and healthcare professionals
Greater awareness is needed around obesity and the associated health risks. That includes addressing the stigma of obesity being a lifestyle issue and informing better decision-making on different treatment options and interventions. This can be accomplished across multiple touchpoints:
- Robust data on health risks and obesity can form the basis for medical journal articles, blog posts, and other publications
- Improved education and training for clinicians, including mandatory obesity modules in medical school, can lead to more informed decision-making
- A multi-pronged outreach campaign utilizing websites, apps, social media, traditional advertising, and public health campaigns can reach a broad audience of consumers and healthcare professionals
- Hosting nutrition workshops and obesity education in schools, as well as collaborating with advocacy groups can lead to enhanced community outreach
- Community as well as online guidance as well as motivational support for behavior and lifestyle improvements
Payers and regulators
Payers and regulators need to provide greater access to digital tools, behavioral support, and other complementary services. Health authorities should also take a more proactive role in providing access to interventions like GLP1s. There are signs that health systems are open to adopting this approach — the UK is spending £20 million to fund research to develop technologies and fast-track access to obesity treatments. The aim is to put a dent in the estimated £6 billion of healthcare costs associated with obesity.
A data-driven and evidence-based approach is key - overweight and obese patients should be enrolled in registries to help understand how different patients benefit from interventions and pave the way for better evidence-based personalization of treatments.
As they flesh out their strategies, payers and regulators should consider these four approaches:
- Embrace complementary services like digital tools that support diet and exercise. Broaden insurance policies that incentivize healthy lifestyle, and subsidize weight management programs
- Expedite approval and reimbursement of innovative drug treatments, implement policies that support drug availability, and negotiate cost-effective pricing
- Establish comprehensive patient registries, leverage machine learning to predict treatment success, and collaborate with research institutes to create real-world evidence
- Allocate funding to improve obesity therapies, create grant programs to grow start-ups, and support public-private partnerships
Digital therapeutics, medtech, and pharmaceutical companies
Manufacturers can enhance their support of patients, healthcare professionals, health systems by advancing data collection and sharing, exploring value-based reimbursement agreements, and investing in the development of ecosystems to provide uniform services to support patients for long-term improvements.
They should take these three actions into account:
- Deploy interoperable electronic health record systems with healthcare professionals, create real-time patient-centered data platforms, and partner with data analytics companies to create insights
- Invest in patient support services, develop digital therapeutics, partner with telehealth providers to enable virtual clinics specializing in obesity care, and participate in industry consortia to establish best practices for digital intervention in obesity management
- Advocate for regulatory policies that increase access to obesity treatments, and collaborate with medical and patient advocacy groups to create awareness for obesity health risks
Tackling the obesity epidemic demands greater collaboration from all sectors of the healthcare industry and eliminating silos. While each segment must balance its own priorities and work through complex business models, unifying around education, data sharing, access to treatment, and more can lead to improved health and reduced costs for patients and society at large.
