Editor's Note: The following industry predictions were first presented via webinar by Welltok and Oliver Wyman.
Some say 2020 is the year that changed everything, but in reality, 2021 will be. What will we learn from this year and how will it change the course of healthcare as we know it?
To help answer these questions, two of the industry’s leading influencers and futurists share their predictions on why this is healthcare’s watershed moment and why change is necessary. Read on for what they had to say about the industry’s most pressing topics.
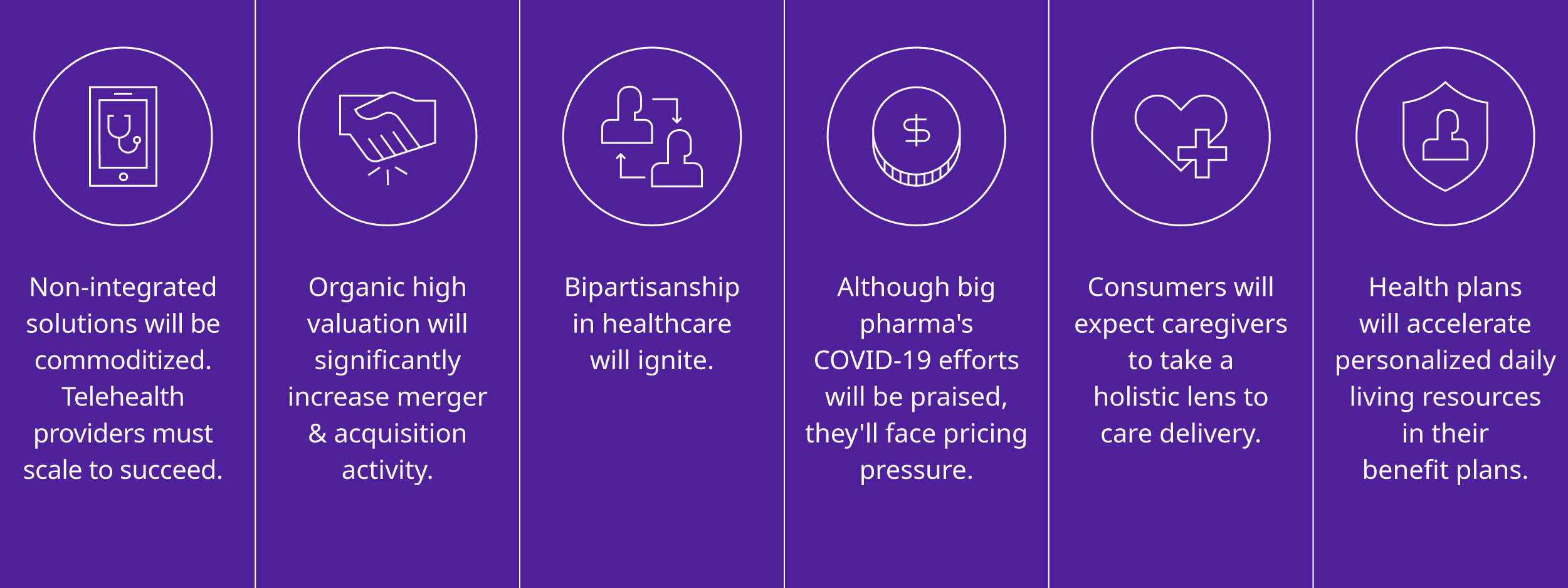
Six Healthcare Predictions for 2021
1. Virtual tele-visit solutions that are not integrated with the consumer’s full healthcare picture will be commoditized. And, growth of telehealth providers who fail to expand beyond traditional clinical visits will decelerate.
Telehealth usage soared during COVID-19 – more so due to convenience over safety concerns. Virtual visits will stick around, but scaling value for consumers will require more than simply putting a provider on a screen. Furthermore, interoperability is a must, so all the information that needs to be integrated into a physical visit must also be accessible and shareable.
“Both physical and virtual visits happen at the speed of people. Digital, which is different than virtual, happens at the speed of computing. We need to create a digital backbone for all interactions by using information technology and higher efficiency ways to change the whole nature of both physical and virtual visits.”
"The level of convenience telehealth offers has staying power. But simply doing a video visit is not going to be enough because it does not harness the power of technology and will quickly become commoditized. Leveraging the power of telehealth for continuous engagement is in its infancy still."
2. Despite partisan challenges, healthcare will be one area where bipartisanship will ignite.
We are going to see more bipartisanship as it relates to healthcare and a general agreement on key agenda items. This is because there is actually a lot of consensus on things like affordability, managed care principles, and that healthcare is a fundamental human right.
“We can argue about the Affordable Care Act and whether it’s going to be repealed and replaced or ruled unconstitutional, but if you really listen through all the noise, there’s general agreement that says there’s a lot of things - preexisting conditions and how long people can be on insurance - that makes sense to everybody. And there are probably ways to incrementally improve it. The mechanism of how you improve it is the political argument.”
“Of all the things that changed between the Obama administration and the Trump administration, the policies that came out of CMS were probably the most consistent. There was a continuous march toward value, a continuous march toward looking at the whole person and changes in reimbursement and transparency. You know, a lot of pro-consumer activity.”
3. Those who have garnered high valuations through organic growth will significantly increase Merger & Acquisition (M&A) activity to achieve and sustain profitability.
With over 45 unicorns (billion-dollar companies) and growing, health tech entrepreneurs are currently getting a lot of attention and interest. This market will continue to grow based on consumer demand, but companies will soon have to shift from the beginning of the funding pipeline to establishing sustainable, profitable models.
“We are in a world right now where the market is awarding high top-line growth, and there’s a lot of imagination around a $3.4 trillion US sick care market. But smart money is going to take their high valuation and strong balance sheets and start looking for real companies that are consistent with their strategy and vision for digital health and technology. They will start conglomerating so they walk out with something that is both efficient on an operational basis, and something that can maintain a reasonable growth rate, where they can grow profitability at a rate faster than the top line.”
“Consumers expect healthcare to look and feel like the rest of their lives, which are increasingly digital. But the current focus on point solutions and a few comprehensive consumer engagement solutions is creating a significant amount of fragmentation. To achieve more sustainable economics, I anticipate high valuation companies will start buying up some of the smaller ones to become bigger players with more profitable growth models.”
4. Big pharma will gain positive recognition for their role in fighting the COVID-19 pandemic, but will, nonetheless, remain subject to massive pricing pressure from governmental healthcare policymakers.
We have finally reached a point where pharm and health plan reputations have turned a corner and consumers have a more favorable view of them. Advancements in data privacy and security have contributed to this shift, as well as the ability to integrate and leverage data to improve the consumer experience. But there is still work ahead for pharma and health plans to solidify favorable reputations.
Furthermore, health plans will successfully skate through a period of higher-than-expected operating margins from lower utilization during COVID-19 and successfully continue to improve their reputations in 2021 and 2022 by visibly supporting vaccinations, increased mental health support, better addressing social determinant disparities, and offering a generally richer benefits set.
“Partly due to COVID, pharma is going to enjoy a moment of sunshine as people acknowledge why so much money has to be spent on R&D by these for-profit companies to improve the human condition through chemistry and biotechnology. But the fact remains that the government and private payers will continue to put pressure on pharma companies for affordable pricing.”
“Health plans are heading in the right direction by moving the right holistic resources toward people based on their unique needs. Historically, plans have been in the ‘no business’, which is how our adversarial system was set up. As they get closer to individuals through better data and vertical integration, they can direct the right holistic resources toward people based on their unique needs and social determinants. This leads to more people liking them, and that’s a good thing.”
5. As consumers, people will expect that physicians (and all types of caregivers) have enough information at their fingertips – including Social Determinants of Health (SDOH) – to have a more holistic view of them and arrange healthcare services in a convenient, realistic and easy manner.
The traditional image of primary care has been a person in a white coat. But this is changing as people identify the healthcare system – and its data and technology platforms – as the primary care provider.
“People have the expectation that the platform which knows you is wherever you are. Additionally, when we talk about the concept of SDOH…you must factor in the concept of a healthcare navigator or quarterback to adequately and systematically provide support, or I think we actually take a step backwards in the health of people.”
“The primary care physician being a singular person is important to some people, but not as many as it used to be. Instead, people want the system – and everyone who takes care of them in it – to have a holistic view of them, whether it is during a 2 a.m. telehealth visit for a sinus infection or at a retail clinic for a sports physical. When this happens, they can move from place to place, getting care when, where, and how they need it.”
6. Commercial health plans (both fully insured and Administrative Services Only, or ASO), Medicare Advantage, and Managed Medicaid Plans will meaningfully accelerate the attachment of personalized daily living resources (for example, “intelligent ecosystems”) to consumers as part of their benefit plan within current premium pricing constraints or face loss of market share.
We can deliver better healthcare and achieve higher health statuses for individuals and populations at a lower cost by continuing to take a more holistic view. The advancements of data and information technology to leverage SDOH lead to the intelligent curation of the right network for the individual consumer. Bottom line: if plans cannot serve the individual, they cannot serve the population.
“Organizations must get an individual tied to the right combination of clinical and daily living support resources for them, because simply drawing a broad swath based on stereotypical socioeconomic, inequality, or expected privileged data, is not going to work. More technology needs to be applied to match up the individual needs of a consumer and surround them with what I would call an intelligent ecosystem.”
“I’m hopeful we are getting there, and despite the dark times we’re going through, the arc is headed in the right direction. This is where the world has to go, and it is exactly the kind of thing health plans have to do to differentiate themselves and not just be the lowest-cost option.”