Editor’s Note: This article is part of Oliver Wyman's ongoing series about the evolving novel coronavirus (COVID-19) pandemic.
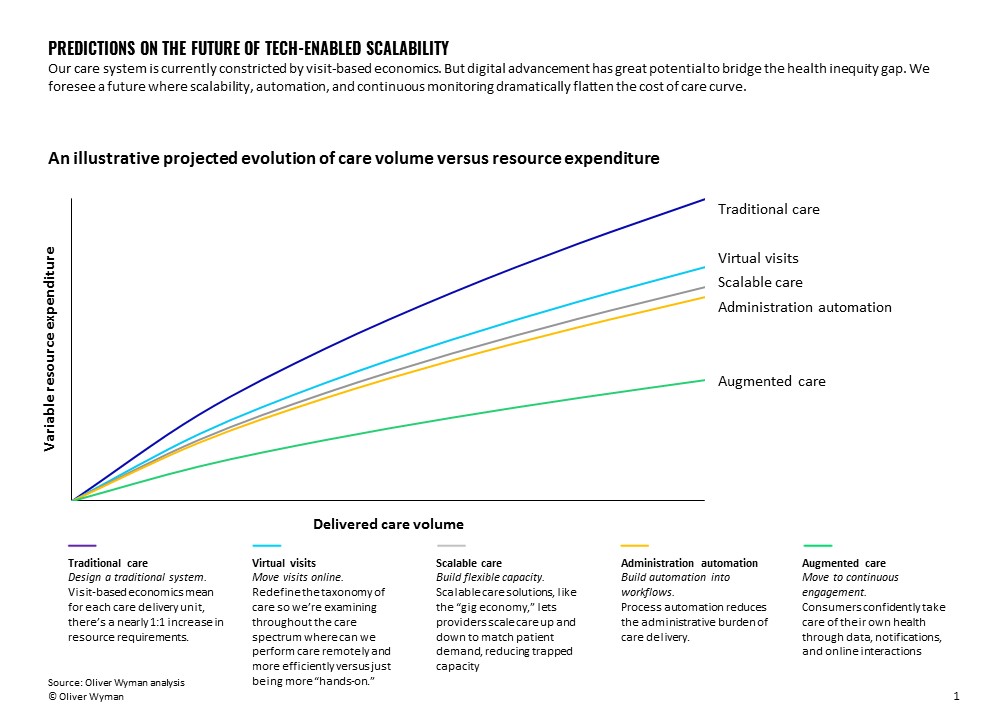
Throughout the COVID-19 pandemic, telehealth visit volume has surged. We envision the future of care will orient away from the traditional, visit-based, and highly resourced constricted system we're used to. It will become more virtual and continuous. Care solutions will be scalable.
It’s easy for providers to be overly focused on telehealth rather than take a broader view on virtual care solutions. But those focused merely on telehealth’s replication of the physical visit will be trumped by those who build scalability and automation throughout the care delivery spectrum.
Capacity
An unintentional, but meaningful, effect of the booming telehealth market is that doctors – now being added to care networks via telemedicine – are new members of a “gig economy.” This creates a powerful lever for health systems to leave their physical spaces lean and scale-up to meet patient demands as needed. The pandemic has led to years of digital advancement and acceptance in the span of months. We're beginning to see the “digital as default” front door of care we’ve envisioned for years. As doctors act as part of the gig economy, we will experience more efficient systems with less vacant spaces and lower costs.
Scalable care solutions parallel how businesses leverage cloud computing. Cloud computing has grown by 3.5 times over the last 10 years. This is as a result of the value businesses see in the ability to rapidly scale computing power in response to their business environment. Surges and droughts in hospital occupancy due to the pandemic have displayed that scalability may be just as vital in healthcare as it’s been in computing.
Automation
Scalability is important but still constricted by traditional visit-based economics where, without redesign, each individual appointment can carry with it an equal amount of administrative burden. Robotic Process Automation (RPA) can reduce variable costs by automating the periphery administrative services associated with delivery care – areas such as back-office billing workflows and customer services
One example of many is Olive, the RPA bot developed by the eponymous Olive.ai. Olive automates business operations in the revenue cycle space, addressing time-consuming and error-prone workflows – including claim status checks and account updates to prior authorizations. In one implementation of Olive, a 2,000-bed health system reduced 300 revenue cycle associates’ work effort of manually checking over 3,500 daily claim statuses and redirecting them to associates. The organization also tripled its revenue cycle team’s efficiency in fewer than five months and realized cost savings of 11 full-time employees. The organization is now positioned to increase the volume of care delivered to its patients without proportionally increasing its back-office costs.
Another vendor doing similar work is Infinitus.ai. They apply artificial intelligence (AI) and RPA technologies to optimize customer service functions in healthcare organizations. Its platform handles large volumes of customer calls by leveraging computer agents that converse in natural language with super-human accuracy. Infinitus’ founders, both ex-Googlers, have improved upon the voice-bot technology first showcased by Sundar Pichai at Google I/O 2018 where a Google robot, mimicking a human, successfully made restaurant reservations by conversing with the restaurant staff. Infinitus claims its voice-bot can hold conversations with humans for up to 30 minutes with minimal errors in context processing and response. While Voice-RPA technologies are still in the early days of implementation, it is easy to see how automating back-office workflows can lead to a reduction in the overall cost structure care delivery.
Looking further into the future, investments in such back-office RPA will become table stakes when operating in a world of continuous care, continuous customer service, and continuous billing.
The scale curve
What do we mean when we talk about next-generation, self-driven virtual care? How is this different than telemedicine, and how does it impact the scale curve?
Here, we are discussing a means of care that will surpass the notion of “visits.” Patient input, remote monitoring, notifications, chat capabilities, AI guidance, and proactive outreach will operate in ensemble as a closed-loop care solution. We anticipate a future where digital is not just an option but rather the default for care.
This may sound like science fiction at first glance, but if you look at the digitization of industries such as retail and banking you will find that customer offerings that at one time seemed to require visits are now predominately digital.
In our earlier Oliver Wyman Health article – Is it Time for a Digital-Only Health System? – our colleagues discussed the parallels between the transition we’re seeing today towards digital care and the transition towards “telebanking” 30 years ago. Today, non-physical access modes are the first choice for most consumers when it comes to their banking needs and we project a similar trajectory for healthcare.
Some innovators are already pioneering the way towards digital-first, continuous care solutions. 98point6, for example, offers on-demand text-based primary care. The application leverages AI to gather pertinent patient information upfront in order to optimize the use of a physician’s time. Babylon Health offers continuous care solutions including AI-powered chatbots, nudges for healthy behavior, health reporting, and a capability to escalate to on-call physicians. Livongo, as another example, offers connected blood glucose meters, smart scales, and on-call expert support as to create a continuous care ecosystem.
Solutions like these are beginning to push the needle towards continuous care ecosystems. These “digital-first” systems leverage tools to empower patients to proactively manage their own care and optimize for efficient use of physician time. The notion of “digital-first” is still in its infancy and will continue to further empower patients and use live physician time more efficiently.
The continuity of these solutions delivers more value and drives down the variable cost of care for each patient. Continuous care solutions enable monitoring and proactive nudges to patient health during their day-to-day lives while traditional care is limited to only small windows into patient health via visits. Meanwhile, the empowerment of patients to manage their own health with digital tools drastically flattens the cost curve since the marginal cost of automated self- service care is close to zero.
Inequity
Minority populations are broadly experiencing disproportionally worse COVID-19 outcomes and health outcomes. New York City in particular identified death rates among Black and African American persons to be 92.3 per 100,000 population versus 74.3 for Hispanic/Latino persons, and 45.2 for White persons. COVID-19’s uneven impact on racial minorities in tandem with the Black Lives Matter movement has put more focus on health inequity now than ever before.
Digital-first, virtual care solutions have the potential to either widen or narrow the gap for low-income communities depending on how policymakers, payers, health systems, and other relevant parties proceed.
Historically, we’ve seen that with advancement, minorities and lower-income persons are often left behind. Pew research data shows that in 2019 the percentage of adults in the US using home broadband is 79 percent for White adults, 65 percent for Black adults, and 61 percent for Hispanic adults. Pew research data shows similar disparities for internet usage overall and internet usage segmented by income. Technology disparities have already presented with virtual healthcare as well. Thomas Sequist, Chief Patient Experience and Equity Officer at Mass General Brigham Hospital, reported only 10 percent of patients in Chelsea, a predominately working-class Latinx community near Boston, used video for teleconsultations. In comparison, over 50 percent of patients from other Boston-area cities were able to use video for teleconsultations. With digital advancement, care accessibility for low-income communities may be inhibited by a lack of access to digital technologies and broadband coverage.
Alternatively, digital-first, virtual care may offer accessible, low-cost care options for many minority and low-income persons. The prevalence of internet usage in the US is high even for lower-income individuals (82 percent for adults with annual income <30K) but could certainly improve. Initiatives such as the Digital Health Connectivity Project are working to empower vulnerable populations with telehealth access. Assuming internet connectivity, virtual care is a much lower cost care option. Babylon Health partnered with the Rwandan government to serve over 30 percent of its adult population. Additionally, low-income and minority persons that do not directly experience the benefits of virtual care should still be able to experience pass-on savings from private and government payers because of the nationwide cost of care reductions.
As Digital Capabilities Advance Amidst COVID-19, Focus on Technological Disparities
Building a digital foundation that enables scalability through current and future pandemic waves – while reducing racial and socio-economic disparities – is beyond critical.
If we take the opportunity to redesign care delivery to maximize our digital capabilities, we might actually make care more affordable and consistently high quality.
