Behavioral health – a complex and multifaceted problem – has taken a back seat to physical health for quite some time. But behavioral health has progressively risen to the top of the list of strategic priorities for many plans and provider organizations. These organizations are now recognizing behavioral health’s tremendous impact on clinical outcomes and overall cost of care, especially as significant investment dollars in the behavioral health space and greater clinical research efforts have further sparked greater recognition of the importance of addressing behavioral health.
Despite elevated interest in this space, much work is yet to be done, and the optimal “solution” remains unknown. We believe there are five key steps toward solving this challenge:
- Acknowledge and agree that behavioral health matters and that addressing behavioral health can have tremendous impact for patients, providers, and payers
- Recognize there is no “one right solution” and transition to a “suite of solutions” approach
- Assemble the right solution set to meet all patient population needs
- Match patients with the optimal treatment solution(s) and ensure engagement and access to high quality care solutions
- Develop systems and processes to monitor condition dynamics and make real-time adjustments to selected solution
In an upcoming series of articles, we will explore these five steps in more detail on the path to solving behavioral health. In this piece, we explore the first two of these critical steps
Step 1: Acknowledge and agree that behavioral health matters and that addressing behavioral health can have tremendous impact for patients, providers, and payers.
Behavioral health is increasingly accepted as a major comorbidity of medical health and a significant driver of overall cost of care. This is critical, as mental health disorders affect nearly 1 in 5, or nearly 44 million, US adults each year. Coexistence of medical and behavioral health conditions results in significantly poorer medical outcomes, adherence to medications and lifestyle measures, greater medical utilization and between two to four times greater total cost of care. These conditions often go undiagnosed, and even when diagnosed, nearly 50 percent of those with behavioral health issues do not receive adequate treatment.
In aggregate, approximately $90 billion is spent on mental illness annually, but nearly $300 billion is spent annually on incremental costs from avoidable medical expenditures and losses attributable to diminished work productivity when mental health issues are unaddressed.
Increased appreciation of the impact of behavioral health on medical health and the value of addressing these issues from both clinical and financial perspectives has led to substantial increase in investment in the behavioral health space over recent years. Recent reports estimate that since 2013, there has been $625 million in venture capital and private equity investment into companies with innovative solutions to address the behavioral health across a wide spectrum of needs. Thus far in 2017 alone, more than $150 million has been invested across 48 deals.
Step 2: Recognize there is no “one right solution” and transition to a “suite of solutions” approach.
While there may be a tendency to think of behavioral health as a single “space,” we need to be thinking about behavioral health multi-dimensionally. Below, we describe three of the most critical dimensions when thinking about the population, their needs, and potential solutions.
Dimension 1: Clinical Severity of Behavioral Health Conditions
Traditionally, the focus in behavioral health has primarily been on the top percentile of patients with the most severe behavioral health conditions. This particular patient segment tends to drive the highest proportion of spend, representing <5 percent of the behavioral health population but accounting for >50 percent of total behavioral health spend.
These patients may have acute needs requiring in person or inpatient care, tend to need case management, and often require coordination with community-based social services. However, a significant number of individuals with moderate risk behavioral health conditions, often with comorbid medical conditions, falls outside this group and as a result often goes undiagnosed and untreated. In aggregate, this population drives a significant amount of avoidable total medical spend.
Finally, there are individuals with the lowest intensity of behavioral health need (the so called “worried well”), who may require only a low intensity solution, and though large in number tend to be low risk and low cost. As a first step, a comprehensive solution must accommodate the full spectrum of clinical severity.
Dimension 2: Spectrum of Behavioral Health Treatment Options
As in physical medicine, where there are often choices available in selecting an appropriate course of treatment given a particular diagnosis (such as knee surgery vs. physical therapy, or bypass surgery vs. percutanous intervention vs. medical management), there are likewise choices to be made in choosing an appropriate intervention for a particular behavioral health condition.
In mental healthcare, treatment choices include psychiatric care, psychotherapy, phamacotherapy, and education and supportive measures. The American Psychiatric Association and other entities periodically update and release clinical practice guidelines to influence treatment selection on the basis of scientific evidence and expert consensus opinion. A comprehensive solution must incorporate access to a spectrum of treatment options.
Dimension 3: Delivery Modality
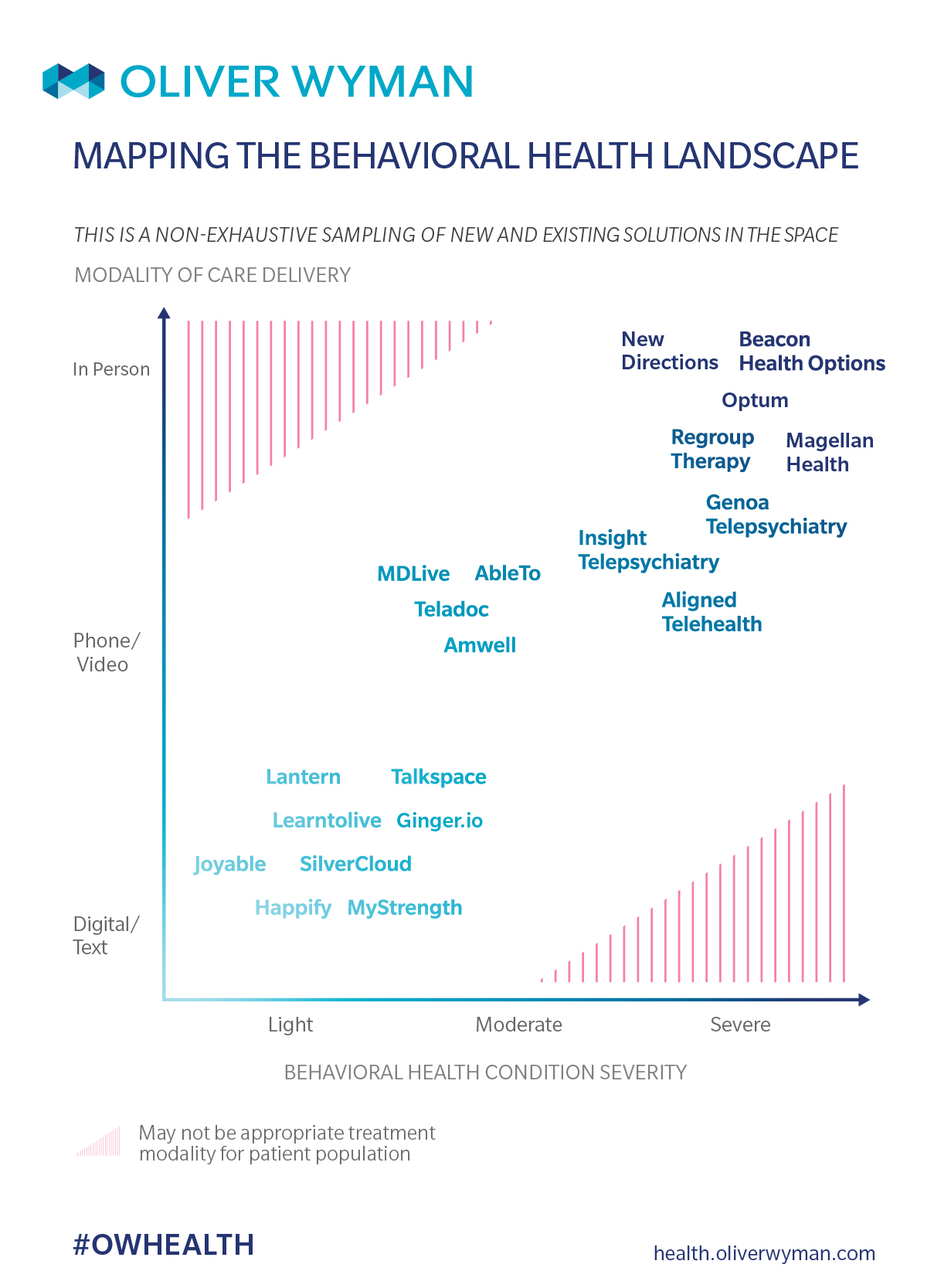
Spurred by the influx of capital into the space and expansive proliferation of technology (like telemedicine, the pervasiveness of smartphones, and artificial intelligence) a broad range of new choices is emerging for how patients receive treatment, support, and education about behavioral health care. These choices create a continuum of intervention options, from light-touch digital solutions with pre-defined content that can be self-navigated at leisure, to more intensive technology-enabled solutions delivered in conjunction with formal coaching and cognitive behavioral therapy, and a plethora of options in between that can supplement (or replace) traditional in-person care.
While on average, choice of intervention correlates with the condition type and severity, there is a growing distribution of appropriate approaches and greatest efficacy that is driven by personal preference, access and other (as yet unknown) factors.
For the same condition, in-person therapy may work best for some patients, while a technology-enabled solution delivered by phone, video, or a purely digital solution may be optimal for others. Moreover, some individuals may benefit from a mutli-modality approach. To meet the needs of this diverse cohort of patients, we must also create access to a range of modalities of treatment for each condition on the severity spectrum.
Recognizing that behavioral health matters and appreciating the value that addressing behavioral health will bring to patients and payers alike is a first key step toward tackling the challenge of behavioral health. Furthermore, we need to acknowledge that behavioral health is complex and multidimensional and that a suite of solutions will be required to meet the needs of patients along a spectrum of disease conditions and severity, recognizing a range of treatment options, and in today’s technological world, a range of delivery modalities.
The emerging ecosystem of new interventions provides more options than have ever existed before. Each is focused on providing a particular modality and intervention to a portion of the population, uniquely positioned to serve a subset of patients. This new ecosystem, when overlaid atop traditional psychotherapy, psychiatry, and pharmacotherapy creates a starting point from which to curate the needed suite of solutions for a particular population.
In our next piece, we will delve deeper on how to assemble the right suite of solutions given the underlying needs of the population and explore how to subsequently match patients with the appropriate solution. We have a tremendous opportunity to lay the groundwork for the optimal solutions set to address the needs of the behavioral health population. Done right, this could have a dramatic impact on improving clinical outcomes and reducing the overall cost of care.