In a previous paper (available here) we discussed the importance of psychosocial wellness and its enormous impact on healthcare costs and outcomes. Patient Activation, a key metric that looks at how patients feel about their health and how involved they are, predicts health outcomes better than ethnicity or age. And the patients at the lowest levels of activation cost the system 8 to 21 percent more than patients with the highest levels of activation. In this paper, we take the next step, and look at how to make wellness metrics the basis of change in the health and social care systems, focusing specifically on the English National Health Service system.
Measuring patient activation
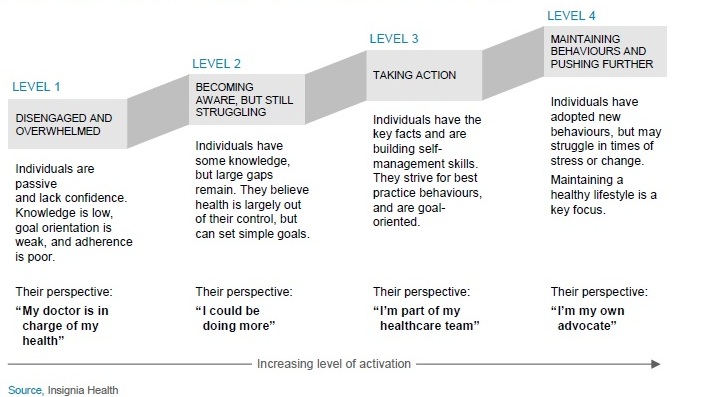
For our purposes, we found that the Warwick-Edinburgh Mental Wellbeing Scale was both feasible and useful in the present landscape in England. Once we understand where patients fall along the activation continuum, we can focus on the practical questions of how to move the patients at level one to level two, the patients at level two to level three, and so forth, using the full range of medical and social institutions, from hospitals to government agencies, workplaces, and schools.
Levels of patient engagement in the Patient Activation Measure