How much impact can a health plan have on whether members perceive it as high quality? What metrics best predict the performance of healthcare delivery systems? Oliver Wyman answers these questions by analyzing the latest round of CMS Medicare Advantage Star Rating scores.
What we learned—that providers have a disproportionate impact on how payers are perceived, that seven CMS metrics are key indicators of quality, and that patients don’t necessarily distinguish between health plan and healthcare provider—contain important lessons for MA plans and offer commercial health plans a valuable glimpse into their own transparent, quality-focused future.
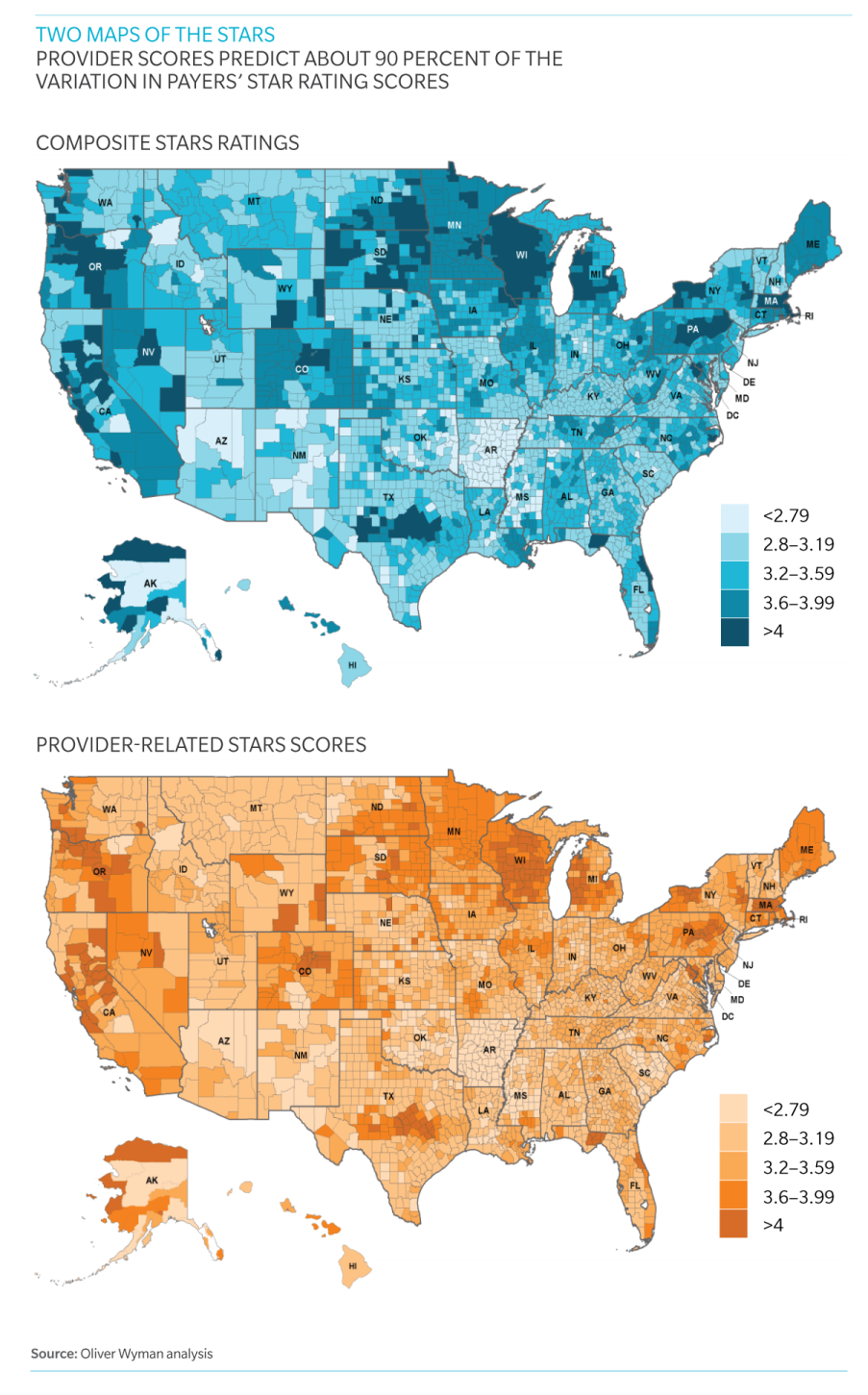
Two Maps of the STARS
To test provider impact on Star Rating scores, we compared average overall scores with average physician scores, all on the county level. The similarities between the two maps show graphically the high correlation between the two. The conclusion: Provider scores predict about 90 percent of the variation in Star Rating scores. Click below to view the maps: