This new report looks at the technological needs of value-based care providers not just today, when care coordination is the primary concern, but tomorrow, when anytime, anyplace becomes the norm and providers work to engage consumers in their own health, and even beyond to a period when data mining and genetic-based predictive modeling bring preventive medicine to new levels of effectiveness. The report includes an assessment of current maturity levels of more than a dozen core technologies.
AN ALTERNATIVE TO THE “BIG SYSTEM” EHR
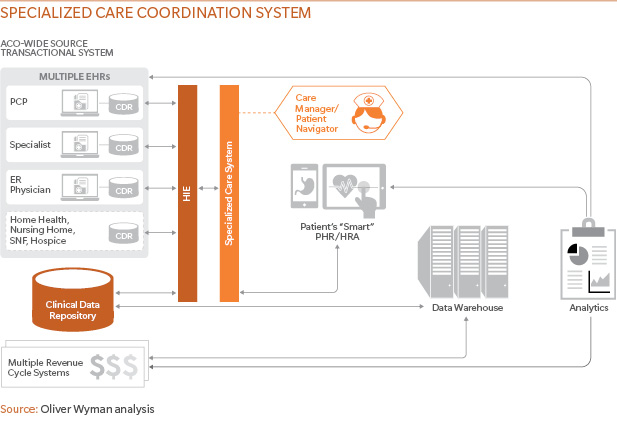
The simple solution to data integration in an ACO is to force everyone to use the same electronic health record. It enables seamless sharing of data, automated workflows, and seamless connections between clinical and financial data. It would be an ideal approach, except that it is expensive, disruptive, and nearly impossible to achieve in a disseminated organization. For many organizations the next-best approach is a specialized care coordination system (CCS) that sits alongside the ACO participants’ existing EHRs. A CCS can be deployed across the ACO at significantly reduced levels of cost, effort, and commitment, because it keeps existing EHRs while allowing integrated care protocols for the populations managed by the ACO. Truth is the EHR is a central link, but no longer the central technology in a fee-for-value environment. See below for an example of a CCS.